
 النبات
النبات
 الحيوان
الحيوان
 الأحياء المجهرية
الأحياء المجهرية
 علم الأمراض
علم الأمراض
 التقانة الإحيائية
التقانة الإحيائية
 التقنية الحيوية المكروبية
التقنية الحيوية المكروبية
 التقنية الحياتية النانوية
التقنية الحياتية النانوية
 علم الأجنة
علم الأجنة
 الأحياء الجزيئي
الأحياء الجزيئي
 علم وظائف الأعضاء
علم وظائف الأعضاء
 الغدد
الغدد
 المضادات الحيوية
المضادات الحيوية|
Read More
Date: 23-2-2016
Date: 23-2-2016
Date: 23-2-2016
|
Thrombosis
Under this topic, we will discuss the definition, pathogenesis, morphology, fates, & clinical significance of thrombi, in this order.
Definition: Thrombosis is defined as the formation of a solid or semisolid mass from the
constituents of the blood within the vascular system during life.
Pathogenesis:
- There are three factors that predispose to thrombus formation. These factors are called Virchow’s triad:
A: Endothelial injury
B: Stasis or turbulence of blood flow
C: Blood hypercoagulability
A: Endothelial injury
- It is the most important factor in thrombus formation and by itself can lead to thrombosis.
- Endothelial injury is particularly important in thrombus formation in the heart & arterial circulation.
- Some Examples:
• Endocardial injury during myocardial infarction & eosinophilic endocarditis in which eosiophils release from their granules crystals called Charcot – Leyden damaging the endocardial endothelium.
• Injury over ulcerated plaque in severely atherosclerotic arteries.
• In hemodynamic stress like severe hypertension & turbulence of flow over scarred valves directly damaging the endothelium.
• Bacterial endtoxin & hyperchloestrolemia, radiation & cigarette smoking may be sources of endothelial injury.
- Irrespective of endothelial damage, the final event is exposure of the highly thrombogenic subendothelial extracellular matrix, mainly collagen & tissue factors up on which platelets undergo adherence & contact activation.
B: Turbulence or Stasis (Alterations in normal blood flow)
Under physiologic conditions normal blood flow is laminar, that is, the cellular elements flow centrally in the vessel lumen separated from endothelium by slowing moving clear zone of plasma. Stasis & turbulence therefore:
a. Disrupt the laminar flow and bring platelets in to contact with the endothelium
b. Prevent dilution of activated clotting factors by freshly flowing blood
c. Retard or make a time lag in the inflow of clotting factor inhibitors and permit the build up of thrombi.
d. Turbulence causes reduction in endothelial PGI2 and tissue-type plasminogen activator (t-PA) which has fibrinolytic activity causing endothelial cell activation. ???
• Stasis is a major factor in the development of venous thrombi while turbulence contributes to arterial & cardiac thrombosis by causing direct endothelial injury or by forming countercurrents & local pockets of stasis.
• Examples:
a) Ulcerated atherosclerotic plaque, which forms a sort of irregularity on endothelial surface, not only exposes subendothelial extracellular matrix but are also sources of local turbulence.
b) Aneurysms are favoured sites of stasis
c) Myocardial infarction not only has endothelial injury but also has a region of noncontractile myocardium, creating an area of stasis resulting in mural thrombus formation.
d) Mitral valve stenosis after chronic rheumatic fever may result in left atrial dilation, usually associated with arterial fibrillation. A dilated left atrium is a site of stasis & a prime location of thrombus development.
e) Hypervisicosity syndrome, i.e an increase in hematocrit in excessive amount due to various reasons such as polycythemia causes stasis in small vessels.
C: Hypercoagulablity
Definition: Hypercoagulability is any alteration of the coagulation pathway that predisposes to thrombosis. Hypercoagulability is a less common cause of thrombosis & & it can be divided into:
1. Primary (Genetic)
- Mutations in factor V[Lieden factor]
- Anti thrombin III deficiency
- Protein C or S deficiency
2. Secondary (Acquired) which, in turn, can be categorized into:
A: High-risk for hypercoagulablity
- prolonged bed rest or immobilization
- Myocardial infarction
- Tissue damage (surgery, fracture, burns)
- ancers (Cancers release procoagulant tissue products to cause thrombosis)
- Prosthetic cardiac valves
- Disseminated intra vascular coagulation
B: Low risk factor for hypercoagulablity
- A trial fibrillation
- Cardiomyopathy
- Nephrotic syndrome
- Smoking
- Oral contraceptives
- Hyperestrogenic state eg. Pregnancy.
Morphology of Thrombi
• Thrombi may develop anywhere in the cardiovascular system.
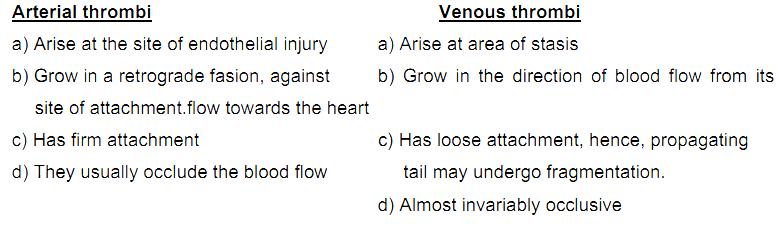
• According to their location, thrombi can be divided into venous & arterial thrombi. (Cardiac thrombi can be considered as arterial thrombi because of certain similarities between the two). The differences between arterial & venous thrombi are:
• The most common site of arterial thrombi in descending order are:
- Coronary arteries
- Cerebral arteries
- Temporal arteries
• Damaged valves can be infected by bacteria or fungi (infective endocarditis) which leads to the development of small infected thrombi on the valves. These small infected thrombi (vegetations) can further damage the valve.
Fates of a thrombus
A thrombus can have one of the following fates:
A: Propagation:
The thrombus may accumulate more platelets and fibrin & propagate to cause vessel obstruction.
B: Embolization:
The thrombus may dislodge and travel to other sites in the vasculature. Such a traveling thrombus is called an embolus. An embolus may obstruct a vessel. The obstruction leads to the death of the tissue supplied by the blood vessel. Death of a tissue due to a decreased blood supply or drainage is called infarction. Therefore, an embolus can eventually lead to an infarction of an organ. E.g cerebral infarction can be caused by a thromboembolus.
C: Dissolution:
The thrombus may be removed by fibrinolytic activity.
D: Organization and recanalization
Organization refers to the ingrowth of endothelial cells, smooth muscle cells, and fibroblasts into the fibrin-rich thrombus. Organization is accompanied by the formation of capillary channels across the thrombus, re-establishing lumen continuity to some extent. This is known as recanalization. The recanalization eventually converts the thrombus into a vascularized mass of tissue which is later on incorporated as a subendothelial swelling of the vessel wall.
Clinical significance of thrombi
• Thrombi are significant clinically because:
- They cause obstruction of arteries and veins &
- They are possible source of emboli.
We will discuss the clinical effects of venous & arterial thrombi separately.
A. Venous Thrombosis (Phlebothrombosis)
Venous thrombosis affects veins of the lower extremity in 90% of cases. It can be divided into superficial & deep vein thrombosis:
1. Superficial venous thrombosis
- Usually occurs in saphenous venous system, particularly when there are varicosities.
- Rarely embolizes
- Causes local edema, pain, and tenderness (i.e. it is symptomatic)
- Local edema due to impaired venous drainage predisposes the involved overlying skin to infection after slight trauma leading to a condition known as varicose ulcer.
2. Deep venous thrombosis (DVT)
- May embolize, hence, is more serious.
- Usually starts in deep veins within the calf muscles.
- Although they may cause local pain & edema, unlike superficial veinous thrombosis, they are entirely asymptomatic in approximately 50% of patients. This is because deep venous obstruction is rapidly offset or releaved by collateral bypass channels.
- Has higher incidence in middle aged & elderly people due to increased platelet aggregation & reduced PGI2 production by the endothelium.
- Has the following predisposing factors:
1. Trauma, surgery, burns which usually result in:-
a:Reduced physical activity leading to stasis
b:Injury to vessels
c:Release of procagulant substance from the tissue
d:Reduced t-PA activity (fibrinolysis)
2. Pregnancy & puerperal states increase coagulation factors & reduce the synthesis of antithrombotic substances. Myocardial infarction & heart failure cause venous stasis to the left side.
3. Malnutrition, debilitating conditions and wasting diseases such as cancer. DVT due to these conditions is known as marantic thrombosis.
4. Inflammation of veins (thrombophlebitis) also predisposes to thrombosis.
5. Migratory thrombophlebitis is a condition that affects various veins throughout the body & is usually of obscure aetiology, but sometimes it is associated with cancer, particularly pancreatic cancer. Migratory thrombophlebitis is also known as Trosseau syndrome.
B. Arterial Thrombosis
- The rapid flow of arterial blood prevents the occurrence of thrombosis unless the vessel wall is abnormal.
- In western society atheroma is by far the commonest predisposing lesion for arterial thrombosis. Atheromatous plaques produce turbulence and may ulcerate & cause endothelial injury, both of which can lead to thrombosis. These thrombi may narrow or occlude the lumen of arteries such as the coronary and cerebral arteries.
Occlusion of these arteries will lead to myocardial infarction (MI) & cerebral infarction respectively.
- Cardiac thrombi can be caused by infective endocarditis, atrial fibrillation,& myocardial infarcion.
- Cardiac thrombosis is common on the heart valves & in the auricular appendages (especially, of the right atrium). A thrombus develops in the atrium in patients with atrial fibrillation & dilatation superimposed on mitral stenosis.
- Myocardial infarction causes dyskinetic myocardial contraction & damage to the endocardium, which usually result in mural thrombi in the ventricles.
- Apart from obstructive features, arterial thrombi (especially, cardiac mural thromi) may embolize to any tissue, but, particularly, commonly to the brain, kidney, & spleen because of large volume of blood flow to these organs.
References
Bezabeh ,M. ; Tesfaye,A.; Ergicho, B.; Erke, M.; Mengistu, S. and Bedane,A.; Desta, A.(2004). General Pathology. Jimma University, Gondar University Haramaya University, Dedub University.



|
|
|
|
دخلت غرفة فنسيت ماذا تريد من داخلها.. خبير يفسر الحالة
|
|
|
|
|
|
|
ثورة طبية.. ابتكار أصغر جهاز لتنظيم ضربات القلب في العالم
|
|
|
|
|
|
|
قسم شؤون المعارف ووفد من جامعة البصرة يبحثان سبل تعزيز التعاون المشترك
|
|
|