
 النبات
النبات
 الحيوان
الحيوان
 الأحياء المجهرية
الأحياء المجهرية
 علم الأمراض
علم الأمراض
 التقانة الإحيائية
التقانة الإحيائية
 التقنية الحيوية المكروبية
التقنية الحيوية المكروبية
 التقنية الحياتية النانوية
التقنية الحياتية النانوية
 علم الأجنة
علم الأجنة
 الأحياء الجزيئي
الأحياء الجزيئي
 علم وظائف الأعضاء
علم وظائف الأعضاء
 الغدد
الغدد
 المضادات الحيوية
المضادات الحيوية|
Read More
Date: 13-3-2016
Date: 9-3-2016
Date: 10-3-2016
|
Treponema (Syphilis, Yaws, Pinta)
Treponema pallidum, subsp. pallidum is the causative pathogen of syphilis. Treponemes feature 10-20 primary spiral windings and can be viewed using dark field microscopy. They cannot be grown on artificial nutrient culture mediums. Syphilis affects only humans. The pathogens are transmitted by direct contact, in most cases during sexual intercourse. They invade the subcutaneous and subserous connective tissues through microtraumata in skin or mucosa. The disease progresses in stages designated as primary, secondary, and tertiary syphilis or stages I, II, and III. Stage I is characterized by the painless primary affect and local lymphadenitis. Dissemination leads to stage II, characterized by polylymphadenopathy as well as generalized exanthem and enanthem. Stage III is subdivided into neurosyphilis, cardiovascular syphilis, and gummatous syphilis. In stages I and II the lesion pathogens can be viewed under a dark field microscope. Antibody assays include the VDRL flocculation reaction, TP-PA particle agglutination, and the indirect immunofluorescence test FTA-ABS. The therapeutic of choice is penicillin G. This disease is known in all parts of the world. Preventive measures concentrate on protection from exposure. Other Treponema-caused diseases that do not occur in Europe include nonvenereal syphilis, caused by T. pallidum, subsp. en-demicum, yaws, caused by T. pallidum, subsp. pertenue, and pinta, caused by Treponema carateum.
The genus Treponema belongs to the family of Spirochaetaceae and includes several significant human pathogen species and subspecies. T. pallidum, subsp. pallidum is the syphilis pathogen. T. pallidum, subsp. endemicum is the pathogen that causes a syphilis like disease that is transmitted by direct, but not sexual contact. T. pallidum, subsp. pertenue is the pathogen that causes yaws, and T. carateum causes pinta, two non-venereal infections that occur in the tropics and subtropics.
Treponema pallidum, subsp. pallidum (Syphilis)
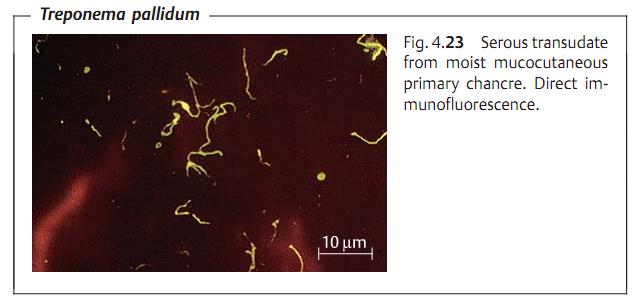
Morphology and culture. These organisms are slender bacteria, 0.2 µm wide and 5-15 µm long; they feature 10-20 primary windings and move by rotating around their lengthwise axis. Their small width makes it difficult to render them visible by staining. They can be observed in vivo using dark field microscopy. In-vitro culturing has not yet been achieved.
Pathogenesis and clinical picture. Syphilis affects only humans. The disease is normally transmitted by sexual intercourse. Infection comes about because of direct contact with lesions containing the pathogens, which then invade the host through microtraumata in the skin or mucosa. The incubation period is two to four weeks. Left untreated, the disease manifests in several stages:
- Stage I (primary syphilis). Hard, indolent (painless) lesion, later infiltration and ulcerous disintegration, called hard chancre. Accompanied by regional lymphadenitis, also painless. Treponemes can be detected in the ulcer.
- Stage II (secondary syphilis). Generalization of the disease occurs four to eight weeks after primary syphilis. Frequent clinical symptoms include mi- cropolylymphadenopathy and macular or papulosquamous exanthem, broad condylomas, and enanthem. Numerous organisms can be detected in seeping surface efflorescences.
- Latent syphilis. Stage of the disease in which no clinical symptoms are manifested, but the pathogens are present in the body and serum antibody tests are positive. Divided into early latency (less than four years) and late latency (more than four years).
- Stage III (tertiary or late syphilis). Late gummatous syphilis: manifestations in skin, mucosa, and various organs. Tissue disintegration is frequent. Lesions are hardly infectious or not at all. Cardiovascular syphilis: endarteritis obliterans, syphilitic aortitis. Neurosyphilis: two major clinical categories are observed: meningovascular syphilis, i.e., endarteritis obliterans of small blood vessels of the meninges, brain, and spinal cord; parenchymatous syphilis, i.e., destruction of nerve cells in the cerebral cortex (paresis) and spinal cord (tabes dorsalis). A great deal of overlap occurs.
- Syphilis connata. Transmission of the pathogen from mother to fetus after the fourth month of pregnancy. Leads to miscarriage or birth of severely diseased infant with numerous treponemes in its organs.
Diagnosis. Laboratory diagnosis includes both isolation and identification of the pathogen and antibody assays.
Pathogen identification. Only detectable in fluid pressed out of primary chancre, in the secretions of seeping stage II efflorescences or in lymph node biopsies. Methods: dark field microscopy, direct immunofluorescence (Fig. 4.23).
Antibody assays. Two antibody groups can be identified:
*Antilipoidal antibodies (reaginic antibodies). Probably produced in response to the phospholipids from the mitochondria of disintegrating somatic cells. The antigen used is cardiolipin, a lipid extract from the heart muscle of cattle. This serological test is performed according to the standards of the Venereal Disease Research Laboratory (USA) and is known as the VDRL flocculation reaction.
*Antitreponema antibodies. Probably directed at T. pallidum.
- Treponema pallidum particle agglutination (TP-PA). This test format has widely replaced the Treponema pallidum hemagglutination assay (TPHA). The antigens (ultrasonically-treated suspension of Treponema pallidum, Nichols strain, cultured in rabbit testicles) are coupled to particles or erythrocytes.
- Immunofluorescence test (FTA-ABS). In this fluorescence treponemal antibody absorption test the antigen consists of killed Nichols strain treponemes mounted on slides and coated with patient serum. Bound antibodies are detected by means of fluorescein-marked antihuman IgG antibodies. Selective antitreponeme IgM antibodies can be assayed (= 19S-FTA-ABS) using antihuman IgM antibodies (i capture test).
- Treponema pallidum immobilization test (TPI test). Living treponemes (Nichols strain) are immobilized by antibodies in the patient serum. This test is no longer used in routine diagnostics. It is considered the gold standard for evaluation of antitreponeme antibody tests.
The antibody tests are used as follows:
- Screening: TP-PA or TPHA (qualitative).
- Primary diagnostics: TP-PA or TPHA, VDRL, FTA-ABS (all qualitative).
- Special diagnostics: VDRL (quantitative); 19S-FTA-ABS.
Therapeutic success can be determined by the quantitative VDRL test. A rapid drop in reagins indicates an efficacious therapy. The 19S-FTA-ABS can be used to find answers to specialized questions. Example: does a positive result in primary diagnostic testing indicate a serological scar or a fresh infection?
Therapy. Penicillin G is the antibiotic agent of choice. Dosage and duration of therapy depend on the stage of the disease and the galenic formulation of the penicillin used.
Epidemiology and prevention. Syphilis is known all over the world. Annual prevalence levels in Europe and the US are 10-30 cases per 100 000 inhabitants. The primary preventive measure is to avoid any contact with syphilitic efflorescences. When diagnosing a case, the physician must try to determine the first-degree contact person, who must then be examined immediately and provided with penicillin therapy as required. National laws governing venereal disease management in individual countries regulate the measures taken to diagnose, prevent, and heal this disease. There is no vaccine.
Treponema pallidum, subsp. endemicum (Nonvenereal Syphilis)
This subspecies is responsible for non-venereal syphilis, which occurs endem- ically in certain circumscribed areas in the Balkans, the eastern Mediterranean, Asia, and Africa. The disease manifests with maculous to papulous, often hypertrophic lesions of the skin and mucosa. These lesions resemble the venereal efflorescences. The pathogens are transmitted by direct contact or indirectly on everyday objects such as clothes, tableware, etc. The incubation period is three weeks to three months. Penicillin is the therapy of choice. Serological syphilis tests are positive.
Treponema pallidum, subsp. pertenue (Yaws)
This species causes yaws (German “Frambosie,” French “pian”), a chronic disease endemic in moist, warm climates characterized by epidermal proliferation and ulceration. Transmission is by direct contact. The incubation period is three to four weeks. Treponemes must be found in the early lesions to confirm diagnosis. Serological syphilis reactions are positive. Penicillin G is the antibiotic of choice.
Treponema carateum (Pinta)
This species causes pinta, an endemic treponematosis that occurs in parts of Central and South America, characterized by marked dermal depigmentations. The pathogens are transmitted by direct contact. The incubation period is one to three weeks. The disease often has a chronic course and can persist for years. Diagnosis is confirmed by identification of treponemes from the skin lesions. Penicillin G is used in therapy.



|
|
|
|
دراسة يابانية لتقليل مخاطر أمراض المواليد منخفضي الوزن
|
|
|
|
|
|
|
اكتشاف أكبر مرجان في العالم قبالة سواحل جزر سليمان
|
|
|
|
|
|
|
اتحاد كليات الطب الملكية البريطانية يشيد بالمستوى العلمي لطلبة جامعة العميد وبيئتها التعليمية
|
|
|