
 النبات
النبات
 الحيوان
الحيوان
 الأحياء المجهرية
الأحياء المجهرية
 علم الأمراض
علم الأمراض
 التقانة الإحيائية
التقانة الإحيائية
 التقنية الحيوية المكروبية
التقنية الحيوية المكروبية
 التقنية الحياتية النانوية
التقنية الحياتية النانوية
 علم الأجنة
علم الأجنة
 الأحياء الجزيئي
الأحياء الجزيئي
 علم وظائف الأعضاء
علم وظائف الأعضاء
 الغدد
الغدد
 المضادات الحيوية
المضادات الحيوية|
Read More
Date: 21-2-2016
Date: 2025-02-13
Date: 2025-02-09
|
Acquired Immunodeficiency Syndrome (AIDS)
- AIDS is a retroviral disease characterized by profound immuno suppression that leads to opportunistic infections, secondary neoplasms and neurological manifestations.
Overview:
- Prevalence: Currently AIDS affects more than 40 million people all over the world and more than 90 % of the infections prevail in developing countries. Currently, the sub- Saharan Africa in general and South Africa, Ethiopia and Nigeria in particular shoulder the greatest burden of this pan endemic.
- Age: Mostly affected individuals are those aged between 15 and 49 years of age however, the epidemiology is quite different in children less than 13 years. Close to 2 % of all AIDS, occur in this age group presently where more than 90 % of this transmission results from transmission of the virus from the mother to the child.
- Sex: Women are more vulnerable than men:
Receptive sexual partners-
• Uterine, cervical and vaginal conditions that promote HIV transmission easily include cervical erosion, cervical ectopy, sexually transmitted diseases (STD), and cervical cancer.
• STD often goes unnoticed due to inaccessible anatomic locations.
• Menstruation: May make the transmission of HIV easier just before, during or after menstruation. It results in a large raw exposed area in the inner uterine lining to the virus
• Those with very low socio economic backgrounds are vulnerable to sex trade (HIV is said to be” the holocaust of the poor”).
• Age of earlier sexual contact where the very young female genital linings are vulnerable to easy lacerations.
Modes of transmission:
- Sexual activities 75% of all world-wide transmission is heterosexual transmission
- Parenteral transmission In intravenous drug abusers, hemophiliacs who received factor viii concentrates and random recipients of blood transfusion
- Mother to child transmission
About 25 –30% HIV, positive mother will transmit HIV to their infants. About 60% of this infection is transmitted during child- birth 25% during pregnancy and 15% during breast-feeding.
- Needle Pricking Accidental needle struck injury or exposure to non-intact skin to infected blood in laboratories accounts for about 0.3% risk of stereovision as compared to a 30% risk of accidental exposure to hepatitis B infected blood.
Etiology:
- HIV causes AIDS and HIV is a non-transforming retrovirus belonging to Lentivirus family. The retrovirus undergoes an unusual biologic process in which the genetic material in form of a single stranded RNA, can be converted to double stranded DNA by the effect of reverse transcriptase.
- Two type of HIV viruses
HIV – 1 - USA, EUROPE, East & central Africa
HIV - 2 - West Africa
- HIV genome consists of a single stranded RNA enclosed within a core of viral proteins. The core is in-turn enveloped by a phospholipids bilayer deprived from the host cell membrane. The Envelop contains glycoproteins such as gp 120 and GP 41, GP 24.
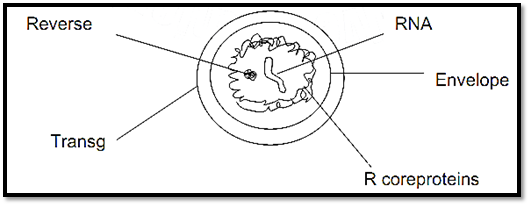
The viral core consists of two protein shells
- The outer contains the core protein P 18 and the inner core protein P 24. The lipid bilayer consists of the viral glycoprotein gp 41 while gp 120 protrudes into the environment. The RNA genome and the reverse transcriptase are contained within the inner shell.
HIV – 1 proviral genome contains 3 genes -Gag – caspid protein P24 , matrix protein P17 , nuclocospial protein P7/9
- Pol - revers trancriptase, protease integrase, ribonuclease
- Env – gp120 and gp41
In addition to these standard genes, the HIV contains other genes including
TAT- Potent transactivator of viral transcription
NEF- Essential for viral replication
REV- regulator of structural gene expression
VIF- Requires for maturation of HIV virus and if also promotes infectivity of cell free virus
VEF- essential for efficient viral replication
VPU- Required for efficient viron budding
VPR Required for viral replication in non-dividing cells and causing viral replication by causing arrest of cycling cells in G2
- On the basis of genetic analysis HIV- I can be divided into two groups designated as M (major) and 0 (outliers). Group M viruses are the most common viruses worldwide and subdivided into several subtypes or clades designated A -J.
- The HIV strains can be classified into two groups based on their absolute to infect macrophage and CD4 + T-cells. Macrophage tropic (M-tropic) stains can infect both monocytes/ macrophages and freshly isolated peripheral blood T-cells. T Tropic strains can infect only T- cells both freshly isolated and retained in culture. M – tropic strains use CCR5 co receptors whereas T – Tropic strains bind to CXCR4 co receptors. Ninty percent (90%) of HIV is transmitted by M – tropic strains, however over the course of infection T – Tropic ciruses gradually accumulate and these are virulent and cause final rapid phase of the disease progression.
Pathogenesis:
- Targets of HIV infections are: The immune system and Central nervous system
- Target cells are those having CD4 receptors include CD4 + T helper cells
Monocytes /macrophages
Tissue cells such as dendritic cells present in genital tracts and anorectal region
Certain brain cells (glial cells)
Some other cells as well
- CD4 - Receptor molecule is a high affinity receptor for HIV. This explains for the selective tropism of the virus to aforementioned cells.
- Initial binding of gp 120 to CD4 molecule leads to conformational change for the new recognition site on gp120 for the co receptors CCR5 or CXCR4.
- The second conformational change in gp41 results in insertion of a fusion peptide into the cell membrane of the target T-cells or macrophages.
- -After fusion, the viral core containing the HIV genome enters the cytoplasm of the cell (internalization).
The life cycle of HIV virus after internalization, include
- DNA Synthesis- the uncoated viral RNA is copied into double stranded DNA by reverse transcriptase
- Viral integration-the DNA derived from the viruses in integrated into host genome by the viral integrate enzyme, thereby producing the latest proviral form of HIV-I.
- Viral replication- viral RNA is reproduced by transcriptional activation of the integrated HIV provirus
- Viral dissemination- to complete the life cycle, nascent viruses assembled in the cytoplasm and disseminate to other target cells after directly lysing the cell (direct cytopathic effect of the virus).
- The HIV virus after internalization assumes two forms of infectivity such as latent infection and productive infections. In latent infections, the virus may be lacked in tne cytoplasm (preintegration latency) or after being integrated into host DNA (Post integration latency). Hereafter the highlight of HIV productive infection is surfaced.
- This productive infection is predominantly occur in lymphoid tissues, within macrophages, dendritic cells and CD4+T CELLS.
- Viremia after 8 weeks of infection supervene
- Viremia is subsequently cleared by the development of an anti viral immune response effected by CD8+cytotoxic T cells
- This results in transient decrease in CD4+T cells and an apparent rise in CD8+T cells
- As viremia declines, the HIV disseminates into lymphoid tissues and undergoes clinical latency but not viral latency
- Finally the ebbs and flows of the CD4+T cells count with variable time results in AIDS.
Mechanisms of CD4 + T cell loss (quantitative defects):
- Loss of immature precursors of CD4 + T cells by direct infection of thymic progenitor cells or by infection of accessory cells that secrete cytokines essential for CD4 + cells differentiation.
- Fusions of infected & uninfected cells with formation of syncythia (giant cells) develop ballooning and these cells usually die in few hours.
- Apoptosis of uninfected CD4 + T cells by binding of soluble gp120 to CD4 molecule.
Qualitative defects on other immune cells as a result of CD4+T helper/ inducer cells loss:
1. Defects of CD4 + T cells:
Reduced antigen induced T – Cell proliferation
- Imbalance between the T-helper 1 (TH1) and TH2 responses favour humoral immune responses over cell mediated immunity
- Decreased lymphokine secretion
T-cell anergy (dysfunction) can also result from the binding of gp120 Ag-Ab complexes to CD4 molecules impairing the antigen presentation by anti -gp 120 antibodies that cross- react with and bind to class II HLA molecule on antigen presenting cells.
Anergy also result from binding of HIV derived suferantigen to B-chains of T-cell receptors.
2. Defects of monocytes / macrophages
These cells are extremely important in the pathogenesis of HIV infection. Similar to T cells majority infected cells are found in tissues not in peripheral blood. A relatively high productive infection of macrophages (10 to 15%) is detected in certain tissues such as Brain and lungs.
1) Several aspects of HIV infection of macrophages include
Hiv-1 can also infect and multiply in terminally differentiated non- dividing macrophages. This property of HIV-1 is dependant on HIV-1 VPR gene.The VPR protein allows nuclear targeting of the HIV pre integration complex through the nuclear pore.
2) Infected macrophages bud relatively small amounts of virus from the cell surface, however, they are quite resistant to the cytopathic effects of HIV.
3) Macrophages in all likelihood act as gatekeepers of infections. More than 90 % of HIV infection is transmitted by M- trophic strains. It has been suggested that macrophages or dendritic cells may be important in the pathogenesis of HIV diseases.
Thus, HIV infection of macrophages has three important implications.
I) Monocytes and macrophages represent a veritable virus factory and reservouir whose output remains largely protected from host defences.
II) Second macrophages provide a safe vehicle for HIV transport to various parts of the body particularly to the central nervous system.
III) In the late stages of HIV, infection when theCD4+T cells numbers decline greatly, macrophages may be the major sites of continued viral replication.
The following are some of the qualitative changes seen in macrophages -Poor capacity of present antigens to T-cells – (most important one)
- Macrophages are quite resistant to cytopathic effects of the HIV
- impaired microbicidal activity,
- decreased chemotaxis
- Decreased secretion of IL-I
- Increased spontaneous secretion of IL-I, TNF - α, IL – 6.
3. B-lymphocyte dysfunctions
- Hypergamaglobinemia and circulating immune complexes
- Inability to mount do novo antibody response to a new antigen
- Decreased immunoglobuline production in response to new antigen
4. Defets of natural killer cells
- Decreased killing of tumour cells
- CD8 + cytotoxic T-cells: decreased specific cytotoxicity, thus, delayed cell mediated immunity
How a latent HIV infection is transformed into productive infection?
- Antigen or mutagen-induced activation of T-cells is associated with transcription of genes encoding the cytokine IL-2 and its receptor (IL-2R) and after some steps induction of nuclear factor- KB (NF– KB) activates the transcription of HIV provirus DNA and leads ultimately to the production of virons and to cell lysis.
- Cellular activation, by antigens or cytokines (e.g.TNF-∞, IL-1, IL-2) induces cytoplasmic kinases that translocate NF-KB from the cytoplasm to the nucleous. In the nucleous, NF-KB binds to the enhancer sequence within the promoter region and similarly long terminal repeats (LTR) have KB sites. Thus, induction of NF-KB
activates the transcription of HIV proviral DNA and leads ultimately to the production of virons and to cell lysis.
- Furthermore, TNF-∞, also leads to transcriptional activation of HIV –m RNA by production of nuclear factors of that bind to KB enhancer elements of HIV.
There are also profound B – cell dysfunctions such as
activation of CMV, and EBV
- Gp41
can also promote B – cell growth and differentiation
- HIV infected cells induce increased production of IL –6 which favours activation of B - – cells
Patients with AIDS are unable to mount antibody response to a new antigen. This could be due to lack of T-cell help. Impaired humeral immunity renders these patients prey to disseminate infections caused by encapsulated bacteria such as S. pneumonia and H.
influenza both of which require antibodies for effective optimization. In totality loss of CD4 + T cells, the master cells, has ripple effect on virtually every other cell of the immune system.
Pathogenesis of central nervous system involvement:
- CNS is a major target of HIV infection. Macrophages and imbroglio are the predominant cell types in the brain that are infected with HIV. HIV is believed to be carried to CNS by infected monocytes, which are almost exclusively of M – tropic type.
Neurons in CNS are not affected directly but indirectly by viral products and soluble factors produced by macrophages / microglia. Included among soluble factors are IL –I, TNF - α and IL – 6. In addition, nitric oxides also induce neuronal damage (according to most investigators).
- Direct damage of neurons by soluble HIV gp120 has also been postulated. According to some investigators these diverse soluble neurotoxins act by triggering excessive entry of Ca2x into the neurons through their action on glutamate – activated ion –channel that regulate intracellular calcium.
Natural history of HIV infection:
Three phases reflecting the dynamics of virus – host interaction are recognized:
I. Early acute phase
High level of viral production, viremia and widespread seeding of lymphoid tissues. Its spread is controlled by immune system and the virus is mainly swept into the lymph nodes The decline in HIV viral load usually coincides with the time of sero-conversion and the primary or early HIV infection. Acute phase occurs 4 – 8 weeks after acquiring the virus There may be a short (1 – 2 weeks) seroconversion illness which cause the following in about 50-70% individuals: fever, rash sore throat, muscle and joint pain and some lymph node swelling. The level of viral load in early acute phase of the disease is called the set point and anti retroviral therapy can reduce this set point thus, early detection especially in cases of needle stick injuries, rape and other known risky exercises can benefit from it.
II. The middle chronic phase
Relative containment of the viruses with a period of clinical latency (not viral latency). Patients develop asymptomatic infections. Persistent generalized lymph adenopathyes (PGL) develops and PGL is defined as palpable lymphodenopathy at two or more extra –inguinal sites, persisting for more than 3 months in persons infected with HIV. Minor opportunistic infections such as trush, herpes zoster etc.
III. The final, crisis phase
Characterized by breakdown of host defences with increased plasmal viral load and clinical disease. Typically the patient presents with Prolonged fever > 1/12 Fatigue, weight loss and diarrhea CD4 + T cells < 500 /μl
After a variable period:
(i) Serious opportunistic infections, (Bacterial, Fungal, Viral
(ii) Secondary neoplasms: Kaposi sarcoma, Non Hodgkin’s lymphoma, Cervical carcinoma
(iii) Clinical neurological diseases (AIDS defining disease)
Case definition of AIDS according to Centre for disease control (CDC)
Any HIV infected person with fewer than 200 CD4 + T-cells /μl + is considered to have AIDS. HIV infection progress to AIDS within 7 to 10 years in most cases, however exceptions to this typical course also occur:
- Long term non progresses
- Those who stay symptomatic for 10 years or more with stable CD4 + T-cells count and low plasma viremia
- Rapid Progresses
- Groups of patients with the middle chronic phase is telescoped to 2-3 years after primary infection
Phases of HIV infections and corresponding CDC classification categories

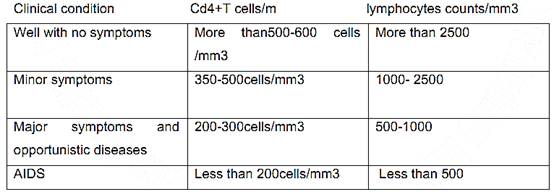
The relationship between the immune status, the CD4+ T cell count, the lymphocyte count, and the presence of symptomatic disease:
References
Bezabeh ,M. ; Tesfaye,A.; Ergicho, B.; Erke, M.; Mengistu, S. and Bedane,A.; Desta, A.(2004). General Pathology. Jimma University, Gondar University Haramaya University, Dedub University.



|
|
|
|
دخلت غرفة فنسيت ماذا تريد من داخلها.. خبير يفسر الحالة
|
|
|
|
|
|
|
ثورة طبية.. ابتكار أصغر جهاز لتنظيم ضربات القلب في العالم
|
|
|
|
|
|
|
سماحة السيد الصافي يؤكد ضرورة تعريف المجتمعات بأهمية مبادئ أهل البيت (عليهم السلام) في إيجاد حلول للمشاكل الاجتماعية
|
|
|