
 النبات
النبات
 الحيوان
الحيوان
 الأحياء المجهرية
الأحياء المجهرية
 علم الأمراض
علم الأمراض
 التقانة الإحيائية
التقانة الإحيائية
 التقنية الحيوية المكروبية
التقنية الحيوية المكروبية
 التقنية الحياتية النانوية
التقنية الحياتية النانوية
 علم الأجنة
علم الأجنة
 الأحياء الجزيئي
الأحياء الجزيئي
 علم وظائف الأعضاء
علم وظائف الأعضاء
 الغدد
الغدد
 المضادات الحيوية
المضادات الحيوية|
Read More
Date: 10-11-2015
Date: 10-11-2015
Date: 10-11-2015
|
Genetic and Population Screening
INTRODUCTION
Genetic testing is defined at the use of specific assays to determine the genetic status of individuals already suspected to be a high risk for a particular inherited condition. Genetic screening uses the same assays to screen a target population. Screening can be defined as the systematic search of populations for persons with latent, early or asymptomatic disease. Screening separates apparently healthy individuals into groups with either a high or low probability of developing the disease for which the screening test is being used. Screening is carried out at various levels. These include maternal prenatal screening, newborn screening, screening for heterozygotes and screening of presymptomatic individuals for specific types of cancer.
REQUIREMENTS FOR POPULATION SCREENING
A genetic population screening program is a systematic attempt to identify and counsel as many people at genetic risk in a population as possible. Genetic population screening requires the highest standards of diagnosis, quality control, information, information and counseling.
The general requirements can be summarised as follows:
•A common and potentially serious condition
•A clear diagnosis
•A knowledge of the natural history of the conditions which will permit correct prediction of outcome
•An effective and acceptable solution in the form of treatment of prevention
•Affordable tests for screening
•The program should be socially and ethically acceptable
• The tests must have a high sensitivity and specificity
Sensitivity and specificity
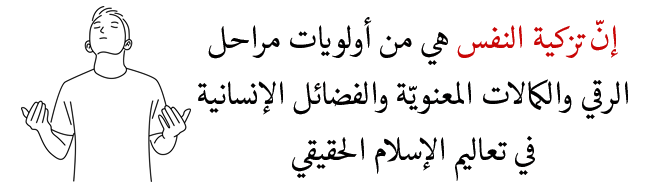
The sensitivity and specificity of a test can be measured as follows:
Sensitivity = a/a+c
Specificity = d/b+d
a = the number of individuals with disease whose screening tests are positive (true positives). c = the number of individuals with disease whose screening test are negative (false negatives). d = the number of individuals without disease whose screening tests are negative (true negatives). b = number of individuals without disease whose screening tests are positive (false positives).
Sensitivity is defined as the ability of the screening test to correctly identify individuals who truly have disease. Specificity is the ability of the screening test to correctly identify individuals who truly do not have disease.
Positive Predictive Value (PPV) is the test’s ability to identify those individuals who truly have disease (true positives) among all those individuals whose screening tests are positive. PPV = a/a+b
Negative Predictive Value (NPVividuals whos) is the test’s ability to identify those individuals who truly do not have the disease (true negatives) among all inde screening tests are negative. NPV = d/c+d
Ethics of screening
1- The program must be voluntary with subjects being offered the screening. If they wish to be screened, informed consent should be taken.
2- Individuals who have positive results on screening should not be pressured into a particular course of action such as prenatal diagnosis or termination of affected pregnancies.
3- The privacy of the individual should be respected and information should be confidential. Countries with insurance based health care systems may have a problem about confidentially of data and the access of such information to their insurance companies providing healthcare insurance.
MATERIAL SERUM SCREENING
Alpha Feto Protein Estimation (AFP) and Triple Test
Maternal serum AFP (MSAFP) levels are raised above the base line in pregnancy due to transfer of AFP across the placenta and amniotic membrane. The concentration of MSAFP rises continuously throughout pregnancy, reaching a peak level at 20 weeks and then decreases. There is an association between elevated amniotic fluid AFP (AF-AFP) and open neural tube defects. However, it would not be feasible to perform AF-AFP as a screening test for NTD. Estimation of AFP in maternal serum was a more practical method. (MSAFP) levels more than twice the median value (>2 MOM) at 16-18 weeks of pregnancy can be used to detect 90% of the affected fetuses. This allowed the development of an effective screening program in UK since mid 1972. Prenatal screening by MSAFP can also provide information on other fetal abnormalities or pregnancy complications (Table.1), which may be associated with elevated MSAFR The significance of low MSAFP along with raised levels of beta hCG and low estriol has been reported to be more predictive with reference to Down’s syndrome and is now routinely used as a screening method to pick up high risk pregnancies for Down’s syndrome. For calculating the risk maternal age, weight, diabetic status and exact gestational age is taken in to account. A combination of Triple Test with increased nuchal thickness on ultrasound can pick up to 85% of at risk babies for Down’s syndrome. Thus, a single specimen of blood taken at 16 -18 weeks can be used to screen for Down’s syndrome and open neural tube defects.
Table.1: Conditions associated with high levels of MSAFP

Obstetric ultrasound
Ultrasound examination in pregnancy is offered as a routine test in pregnancy in most centres, deally done at 18 weeks gestation, is valuable in picking up some markers of fetal chromosomal disease. The diagnosis needs to be confirmed by invasive foetal tissue sampling procedure, And is described in details in chapter on prenatal diagnosis.
Newborn screening
Newborn screening involves the analysis of blood or tissue samples taken in early infancy in order to detect genetic diseases for which early intervention can avert serious health problems or death.
Principles of newborn screening
1- The disorders screened for are those in which symptoms would not be clinically present until irreversible damage occurred and for which there is an effective treatment.
2- There is a prevalence of the disorder in the population.
3- Collection of the sample is by a simple collection method.
4- The results are reproducible with few false positives and negatives.
5- There is a high benefit-to-cost ratio.
6- Abnormal results can be followed up.
Specimen Collection
The specimens used are usually dried filter paper blood spots, and the infant is < 72 hours of age and preferably after 24 hours of protein feeding.
In the United States, newborn screening is carried out for the following disorders: PKU, congenital hypothyroidism, galactosemia, maple syrup urine disease, homocystinuria, biotinidase deficiency, sickle cell disease, tyrosinemia, congenital toxoplasmosis, congenital adrenal hyperplasia, and cystic fibrosis. Some of these are discussed below.
pku
The enzyme deficiency in PKU is phenylalanine hydroxylase, causing failure in conversion of phenylalanine to tyrosine. The incidence is 1:12,000 live births in USA. Accumulation of phenylalanine in classic PKU is > 20 mg/dL with normal or reduced level of tyrosine. Atypical PKU is 12-20 mg/dl, and mild persistent hyperphenylalaninemia has levels of 212 mg/dl. Treatment is a phenylalanine restricted diet instituted by 3 weeks of age, and frequent monitoring of blood levels and diet adjustments. Early treatment prevents mental retardation and neurologic abnormalities, although learning disabilities are still present. Continuation of diet indefinitely is recommended to prevent decreases in IQ and maternal PKU, which results in fetal microcephaly, congenital heart disease, and IUGR.
Congenital Hypothyroidism
The incidence in the USA is 1:3,600-5,000 live births. Screening is by measurement of T4/TSH. Symptoms include mental retardation, neurologic abnormalities and metabolic symptoms of hypothyroidism. Treatment involves administration of L-thyroxine to maintain T4 levels in the upper half of the normal range. Treatment within the first 3 months of life is associated with prevention of mental retardation and complications of the disease
Galactosemia
The prevalence is 1:40,000 live births. Caused by deficiency of galactose-1-phosphate uridyl transferase. Screening is by measurement of galactose and galactose-1-phosphate, and confirmation is by measurement of the enzyme in erythrocytes. Treatment includes dietary lactose restriction at time of diagnosis, evaluation for sepsis, and immediate treatment to prevent complications of mental retardation, cataracts, and cirrhosis.
Sickle Cell Disease and other Hemoglobinopathies
These include hemoglobin SS disease, hemoglobin SC, and sickle-thalassemia, all of which result from abnormal P-chains of hemoglobin. The incidence in the black population is approximately 1:400. Screening is by hemoglobin electrophoresis by using cord blood or dried filter paper blood spot.
Glucose-6-phosphate Dehydrogenase Deficiency
The incidence is 1:100-1:10 for Mediterraneans, Africans and American Blacks, and 1:50-1:33 for Southeast Asian individuals. This is a sex-linked disorder primarily affecting males, although females may be variably affected. It is a hemolytic disorder, where enzyme deficient RBCs are unable to protect against oxidative effects of infection or certain drugs resulting in severe haemolysis and hyperbilirubinemia. Screening is by a fluorescent spot test, which measures the absence of the enzyme. The diagnosis is confirmed by quantitative analysis.
Congenital Adrenal Hyperplasia
This is an autosomal recessive disorder of the biosynthesis of adrenal corticoids due to a deficiency of one of several enzymatic systems required for complete steroid biogenesis. Most common form of CAH is due to 21-hydroxylase deficiency (90% of cases), in 2/3 there is increased androgen production. The incidence is 1:10000-1:15000 live births. The screening test measures level of 17-hydroxyprogesterone in the dried filter paper blood spot. Early treatment will prevent complications seen in undiagnosed affected newborns, and incorrect sex assignment in females.
Maple Syrup Urine Disease
This disorder is due to deficiency of branched-chain ketoacid dehydrogenase that results in the accumulations of the branched-chain amino acids leucine, isoleucine and valine and their respective ketoacids. The incidence is 1:200,000 live births. The screening tests for leucine by the bacterial inhibition assay on dried blood filter paper. Treatment consists of diet restriction.
Homocystinuria
This is due to deficiency of cystathionine synthase that catalyses the conversion of homocysteine to cystathionine, and results in accumulation of toxic levels in blood or urine. The incidence is 1:100,000-1:200,000. The screening test measures methionine in dried filter paper specimen. Treatment includes a methionine-restricted diet.
Cystic Fibrosis
The incidence is 1:2000 in the Caucasian population. Screening is by measurement of immunoreactive trypsin (IRT) in the dried filter paper blood spot. Affected newborns have elevated levels. A second test is usually requested in 2 weeks if first is positive. If the second test is positive, infant referred for sweat test for definitive diagnosis.
Population screening for heterozygotes
Carrier screening identifies individuals with a gene or chromosome abnormality that may cause problems either for the offspring or person screened the testing of blood can indicate the existence of a particular trait that is associate with inherited disease in asymptomatic individuals.
The following aspects need to be considered before population screening for heterozygotes:
1-Information about the frequency, etiology, symptoms, course and therapeutic possibilities for the disease for which heterozygosity is determined should be known and available. Upon obtaining complete information the individual to be tested should provide informed consent.
2-If heterozygosity is demonstrated comprehensive counseling of the significance of results is required. This is necessary to prevent false judgements leading to discrimination and stigmatisation.
3-If two partners are heterozygotes they should be informed about the risks of their offspring inheriting the disease. They should be offered all options including accepting the genetic risk and offspring with the disorder, prenatal diagnosis, termination of theaffected pregnancy of adoption and the couple should be allowed to make an informed unpressured decision.
An example for implementation of carrier screening includes the hemoglobin disorders (Fig. 1). Between 3-20% of most populations carry the sickle cell trait or thalassemia. Carriers can be identified by simple methods and carrier screening is accurate. Prevention programs are treatable and cost effective. An example of such as effective screening program involves the control of thalassemia in Cyprus. Each year 5000-8000 children are born with Thalassemia major. Epidemiological studies have shown that the problem is largely observed in India in certain communities like the Sindhis, Khatris, and Kutchis as well as in Marathas in Maharashtra. A number of teaching hospitals and NGO’S have taken up population screening, and the effect of this may be seen in the coming years. Other conditions include screening for cystic fibrosis in the Caucasian population and screening for Tay-Sach’s disease is the Ashkenazi Jewish population.
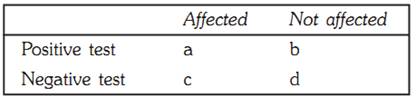
Prenatal diagnosis of P-thalassemia is successfully achieved in the first trimester by chorionic villus sampling. The technique is DNA based diagnosis (Fig. 2).
Fig. 1: The beta globin gene map showing some common mutations. The lower half shows agarrose gel electrophoresis of products generated using the ARMS technique. Courtesy Dr. John Old, National Hemoglobinpathy reference Center, Oxford, UK

Fig. 2: Prenatal diagnostic evaluation for a mutation on a CVS sample. The Analysis of lane 4 using the ARMS technique shows that the fetus carries the trait and is not affected
PRESYMPTOMATIC SCREENING OF ADULTS
Presymptomatic screening of adults is carried out for family members with a history of autosomal dominant conditions with delayed onset of symptoms. Examples include screening for adult polycystic kidney disease using renal ultrasound and DNA studies, and screening for von Hippel-Lindau disease using cranial and abdominal CT scans and DNA studies. This permits genetic counseling of affected individuals and maybe necessary for effective therapy, and example of which includes early removal of tumours in Von Hippel Lindau disease or colectomy prior to the development of cancer in polyposis coli.
Prevention and screening for some adult genetic disorders
1- Breast cancer screening is carried out using mammography and physical examination of the breast. Monthly selfexamination are recommended for all women and mammograms every 2-3 years for women 40-50 years old. For patients with familial breast cancer mutation screening of the BRCA1 and BRCA2 genes can be carried out.
2- Screening for colorectal cancers is by testing the stool for occult blood. Endoscopy for high-risk individuals over 50, and target populations for screening include individuals with a history of colitis, familial polyposis or adenomas, and familial cancer of the colon. The screening test for such individuals includes sigmoidoscopy, ophthalmoscopy and DNA studies.
3- Screening for cervical cancer is using the Pap smear to detect cervical abnormalities every 1-3 years beginning with when the woman first becomes sexually active.
4- Screening for prostrate cancer is by digital palpation of the rectum and serum acid phosphatase concentration. The target population includes men aged 65 and above.
Principles of Population Screening for Cancer
The purpose of population screening is to divide eligible subjects into 2 groups. Those with a low risk of having cancer, and those with a sufficiently high risk to warrant further diagnostic examination. Screen is applied to asymptomatic individual and the goal is to identify individuals whose disease is at preclinical stages so it can be effectively treated.
An ideal carrier screening program will have the following attributes:
References
Purandarey, H. (2009). Essentials of Human Genetics. Second Edition. Jaypee Brothers Medical Publishers (P) Ltd.



|
|
|
|
4 أسباب تجعلك تضيف الزنجبيل إلى طعامك.. تعرف عليها
|
|
|
|
|
|
|
أكبر محطة للطاقة الكهرومائية في بريطانيا تستعد للانطلاق
|
|
|
|
|
|
|
العتبة العباسية المقدسة تبحث مع العتبة الحسينية المقدسة التنسيق المشترك لإقامة حفل تخرج طلبة الجامعات
|
|
|