
 النبات
النبات
 الحيوان
الحيوان
 الأحياء المجهرية
الأحياء المجهرية
 علم الأمراض
علم الأمراض
 التقانة الإحيائية
التقانة الإحيائية
 التقنية الحيوية المكروبية
التقنية الحيوية المكروبية
 التقنية الحياتية النانوية
التقنية الحياتية النانوية
 علم الأجنة
علم الأجنة
 الأحياء الجزيئي
الأحياء الجزيئي
 علم وظائف الأعضاء
علم وظائف الأعضاء
 الغدد
الغدد
 المضادات الحيوية
المضادات الحيوية| Genetic and Congenital Abnormalities (Dysmorphology and Teratogenesis) |
|
|
|
Read More
Date: 30-10-2015
Date: 10-11-2015
Date: 10-11-2015
|
Genetic and Congenital Abnormalities (Dysmorphology and Teratogenesis)
INTRODUCTION
The development of a human fetus is an extremely complex process and is dependent on genetic as well as environmental factors. Genetic factors contribute to malformations from birth, though they can be expressed anytime during life. The effect of environmental factors or teratogens leading to congenital malformations is dependent on the developmental stage at the time of exposure, the duration of exposure and the dose. The mechanism of the abnormality leading to a structural defect can be studied in animal models. Though diagnosis of congenital malformations may be difficult at times, it is important for genetic counseling for recurrence risk estimation, and for preventive reproductive options.
INCIDENCE
Spontaneous Abortions and Genetics
A large number of conceptuses are lost before implantation at 5-6 days, before a woman realizes that she is pregnant.
Amongst recognizable pregnancies, 15% end in the first trimester, of which 80% have abnormalities either in the form of a blighted ovum or a specific abnormality of a chromosome, namely aneuploidy, trisomy, monosomy or triploidy. It has been observed that genetic diseases and environmental teratogens significantly contribute to the fetal loss rate and malformations. With the extensive use of ultrasound in obstetric care, the term spontaneous abortion is used synonymously with missed abortions. This is because most pregnancy losses are picked up by an ultrasound examination before they are spontaneously aborted. Analysis of abortuses has shown that 50% of early fetal losses are due to chromosomal errors. Evaluation of causes of fetal loss is becoming more important for two reasons. Firstly, a decrease in the average family size and secondly, a delay in maternal age at first conception. This causes an increased emotional focus on each individual pregnancy.
In a fetus as young as 10 weeks gestation, certain morphological abnormalities can be visualized, therefore the fetus should be examined for morphological abnormalities and a co-relation between gestational and developmental age should be made. For example, at 10 weeks gestation the presence of intestines in the umbilical cord is a normal finding (Fig. 1A). If the same condition is observed at a later gestational age, it is classified as omphalocele and could be associated with chromosomal defect like trisomy 18. Another example iscoloboma of the iris (Fig. 1B), which is a normal finding up to the age of 45 days, or cleft lip and palate, (Fig. 1C) which is normally seen up to 10 weeks of development. If these are seen after the above mentioned specific periods, these are labeled as developmental defects.
Many a times in early pregnancy, fetal demise could have occurred several weeks before an actual miscarriage. In such cases, fetal tissue may not be available or may not be suitable for karyotyping.
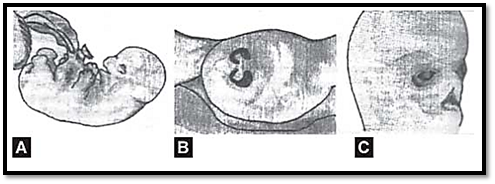
Figs 1A to C: (A) Physiological hernia in a fetus at 9 weeks, (B) Coloboma iris. (C) Cleft lip and palate at 10 weeks
Histopathological studies in early abortions may be of value in early losses. On histopathological examination, markedly hydropic villi with cistern formation indicate a molar gestation. Hydropic villi intermingled with small normal villi are diagnostic of partial mole. Trisomies have slightly hydropic avascular villi. In monosomies chorionic villi differ greatly in shape and are irregular.
In older fetuses it is possible to achieve at a diagnosis by studying the photographs, autopsy reports and X-rays. Such an evaluation is of extreme importance in estimating the recurrence risks and planning a more precise pre-natal diagnosis for future pregnancies.
Perinatal Mortality and Congenital Malformations
Pregnancy losses between 28 weeks and the first week of life fall into this group. 25 to 30% of perinatal mortality is due to a serious structural abnormality, and 80% of these are of genetic origin. Recurrence risk is more than 1%. Many biochemical disorders like amino acidopathies, urea cycle defects and carbohydrate metabolism disorders can prove to be fatal in newborn period and fetal tissues need to be cultured for enzyme assays. A precise diagnosis is necessary for future pregnancy planning.
Ten percent of newborn babies have one to two minor abnormalities. About 2 to 3% of all newborns have some major anomaly presenting at birth and the incidence is about 5% in those which present in later in life. 25% of all deaths in childhood occur due to major structural anomalies. The quality of life in patients with major malformations depends on the nature of the defect and its possible correction. Nearly 25% of the patients with birth defects die in early life and 25% are physically and mentally handicapped.
CLASSIFICATION OF BIRTH DEFECTS
Birth defects are classified into malformations, disruptions, deformities and dysplasias according to the mechanism that has caused the defect. Sequences and syndromes are also identifiable types of birth defects.
Malformations
Malformations are primary structural defects that occur during development of a tissue or an organ. A malformation develops from an abnormality during the course of development. Examples of malformations are cleft lip and palate, congenital heart disease, pyloric stenosis and meningomyelocele. Most of the single gene malformations are polygenic/multifactorial, in origin with a low risk of recurrence. Surgical treatment is recommended for correction. Multiple malformation syndromes comprise of defects in two or more systems and are associated with mental retardation (Fig. 2). The recurrence risk depends on the cause, whether it is chromosomal, teratogenic or a single gene defect or unknown.
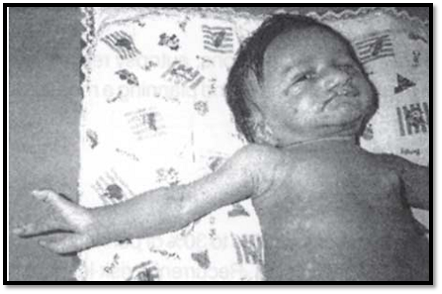
Fig. 2: Multiple congenital anomalies
Disruption
The term disruption is applied to a condition where the fetus has otherwise developed normally, and a disruption in development occurs due to external factors. For example, in amniotic band syndrome, an amniotic band is formed due to early rupture of the amnion and can disrupt a limb, and cause a constriction leading to limb deficiency, classically known as a limb reduction defect (Fig. 3). Interference with blood supply to a developing part leading to infarction or infection can also lead to the defect. Association of limb reduction defects with chorionic villous sampling (CVS) has been reported. Although the occurrence of limb reduction defects after CVS are yet to be investigated, in order to reduce the risk, it is safer to do sampling after 9 V weeks of pregnancy.

Fig. 3: An example of a disruption is the amniotic band syndrome. Here constriction defects seen in the lower limbs due to amniotic bands
Deformations
Deformities due to abnormal intrauterine moulding can arise because of maternal or fetal conditions. Dislocation of the hip joint, and clubfoot result from oligohydramnios. Fetuses with abnormalities of the musculoskeletal system may have positional deformities. Multiple pregnancies or breech presentation can also result in deformities. A well renal recognized syndrome, Potter syndrome (Figs 4A and B) is associated with renal agenesis leading to oligohydramnios, which in turn can cause fetal deformation and pulmonary hypoplasia.

Figs 4A and B: An example of a deformation is the potter syndrome. Note the severe oligohydramnios seen on ultrasound (A) and (B) a fetus with Potter syndrome
Dysplasia
The term dysplasia is applied to an abnormal organization of cells in a tissue and usually affects all parts of the body where that particular tissue is present. An example is thanatophoric dysplasia, which is a type of skeletal dysplasia, which occurs due to mutations in FGFR3 gene (Figs 5A and B). Here all parts of the skeleton are affected. In ectodermal dysplasia, tissues of ectodermal origin like hair, teeth and nails are involved. Most dysplasias occur as a result of single gene defect, and have a high recurrence risk for siblings and children.
Sequence
Sequence is where a single site defect results in apparently unrelated anomalies due to a developmental cascade. For example, in Potters syndrome due to chronic leakage of amniotic fluid or renal agenesis, oligohydramnios occurs which leads to fetal compression resulting in dysmorphic facial features, dislocation of hips, pulmonary hypoplasia and
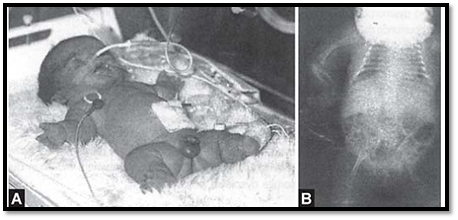
Figs 5A and B: (A) Skeletal dysplasia in a new born (B) X-rays of the same infant showing shortening of the long bones and narrow thoracic cavity
talipus. The condition is invariably fatal. Similarly in spina bifida, blockage in the normal CSF flow can result in hydocephalus (Figs 16.6A and B).

Figs 6A and B: Ultrasound showing. (A) Meningomyelocele and (B) Hydrocephalus occurring secondary to obstruction of the flow of cerebrospinal fluid,an example of a sequence
Syndrome
The term syndrome is applied to conditions where consistent patterns of abnormalities are seen due to an underlying cause. Syndrome is a combination of birth defects that is consistent in unrelated individuals. Many syndromes show some phenotypic variation both in individuals throughout life and between different individuals. This could be due to chromosomal abnormalities as in Down’s syndrome or without any chromosomal abnormality as in Pierre Robin syndrome. Several multiple malformation syndromes are recognized and a computerized dysmorphology data base is now available, which is of great help in evaluating prognosis and estimating recurrence risk.
Association
Association is the non-random association of groups of congenital anomalies but in a relatively inconsistent manner. The recognized malformations have acronyms of the abnormalities, e.g. VATER association comprises of vertebral anomalies, anal atresia, tracheoesophageal fistula and radial defects. The acronym VACTERL is the VATER association but includes cardiac defects and hydrocephalus. CHARGE association includes (coloboma, heart defects, atresia of the choana, retardation of growth, genital anomalies, ear anomalies). Another example is the MURCS association where mullerian duct aplasia, renal aplasia and cervicothoracic somite dysplasia is observed.
Twinning and multiple births
Approximately 7.6% of the pregnancies result in twins, of which 6% vanish and only 1.6% go to term. The rate of malformations is higher in twins. Twins are divided in to two groups - monozygotic (MZ) where twins are identical and are developed from the fertilization of one egg and one sperm (single zygote) within 3-8 days of fertilization. If the division occurs more than two weeks after conception there is a great possibility of conjoined twins. MZ twins usually do not have a family history, have the same genetic composition, are of the same sex though phenotypically they may not be identical. Monozygotic twins sometimes can be discordant for genetic disorders and congenital malformations. MZ female twins can show discrepancy in X-chromosomal inactivation. Dizygotic twins (DZ) are formed when fertilization occurs between two eggs and two sperms in the same ovulatory cycle. They are like sibs and may be of the same or of different sexes. Multiple births occur in a similar fashion. MZ twining is a chance occurrence while DZ twining is familial and has three times increased risk of recurrence. Multiple births like triplets or quadruplets, can be identical or non-identical. Twin studies are of importance in medical genetics. MZ and DZ twins are excellent models for comparative studies of the effects of genes and environment.
Genetic causes of malformations
Many genetic causes of congenital malformations are known and are classified as chromosomal, single gene, and multifactorial.
Chromosomal Abnormalities
Chromosomal abnormalities occur in 6% of all recognized congenital malformation.
Single Gene Defects
7.5% of congenital anomalies occur due to a single gens defect. They can present as isolated defects or can involve multiple systems, and have no embryological relationship. An appropriate classification and mode of inheritance is essential to estimate recurrence risk.
Multifactorial Inheritance
A majority of congenital malformations fall into this group where genetic and environmental factors are responsible. Most isolated malformations of the heart, central nervous system and kidneys are due to multifactorial inheritance. The empiric risks need to be calculated before counseling can be offered for recurrence risk estimation. An example of genetic and environmental components for a defect is described below.
Neural Tube Defects
One of the common developmental defects occurs due to a failure of closure of the neural tube. When the defect lies at the upper end of the tube it leads to anencephaly, and when it lies in the lower region it leads to spina bifida and meningomyelocele. Environmental factors play a great role in the causation of a neural tube defect. Most defects have serious implications leading to incompatibility with life due to anencephaly or paralysis of the lower limbs and loss of bowel and bladder control in spina bifida. Recurrence in patients increases in subsequent pregnancies and is also higher in close relatives. Prenatal diagnosis is by estimating serum a fetoprotein levels in maternal blood. Mothers carrying a fetus with open neural tube defects show a high level of serum alfafetoprotein levels in their blood. Ultrasonography can diagnose the condition in 90% of cases. Prevention in a large number of cases is possible by periconceptional high doses of folic acid. If a neural tube defect is associated with other congenital malformation or part of any other syndrome, the underlying cause has to be evaluated and if suspected to be chromosomal, a chromosomal diagnosis should be offered. Socio-economic factors, multiparity and valproic acid embryopathy also contribute to neural tube defects. Therefore folic acid supplement is recommended for all pregnant women, not only to those with a past history or a positive family history.
Environmental teratogens
An agent which causes a defect in the natural process of development is called a teratogen. The teratogen can be in the form of drugs, chemicals or infections. Organ involvement depends on the nature of teratogens, and the severity of the problem depends on the dose and developmental stage of the fetus.
Drugs and chemicals
Overall 2% of all congenital malformations fall in this group. Various drugs are known to be teratogens, for example anticancer drugs like methotrexate and chlorambucil and anticonvulsants such as carbamazepine and primidone. Minamata disease a disease caused in children who are born to mothers who had ingested organic mercurials through contaminated fish. This is an example of industrial pollution. The babies have a cerebral palsy like syndrome.
Thalidomide was a drug used as a sedative in Europe during 1958-1962 and caused severe limb anomalies in babies whose mothers were exposed to the drug between the 25th to 35th day of conception. This deformity with severe limb defects is known as phocomelia. In a short span, about 10,000 babies were reportedly born. The limb defects consisted of absence of fore or hind limbs, with retention of digits. Other external anomalies like ear, eye cleft lip and palate are also known to occur. 40% of thalidomide babies died in early infancy due to severe internal anomalies of heart, kidneys and gastrointestinal tract.
Fetal Alcohol Syndrome (FAS)
Ethanol ingestion during pregnancy causes congenital malformations and delayed psychomotor development. The clinical features include mental retardation, microcephaly, hypotonia, poor coordination, hyperactivity and impaired growth. The children tend to show a characteristic facial appearance. This includes short palpebral fissures, short upturned nose, hypoplastic philtrum, micrognathia and hypoplastic maxillae. The risk of alcohol-induced birth defects is established above 3 oz. of absolute alcohol daily.
Maternal infections
The process of embryogenesis is affected by maternal infections, and these can interfere with fetal development. The most susceptible organs are brain eyes and ears. A group of infections, seen commonly is called the TORCH group of infections, which stands for toxoplasma, rubella, cytomegalovirus and herpes.
Rubella
Infection with the rubella virus causes malformations in 15% to 25% of pregnancies. Infection in the first trimester causes cardiovascular malformations, cataracts and a hearing defect. Prevention of rubella is possible by immunization of all young women independently or as measles mumps and rubella vaccination together (MMR) and should be included in routine health care and obstetric care programs.
Cytomegalovirus
The cytomegalovirus infection in the first trimester leads to occurrence of congenital malformations in 5% of the infected pregnancies.
Toxoplasmosis
This parasitic infection in pregnancy has a 20% risk of fetuses getting infected in the first trimester, which rises to 75% in the second and third trimester. The diagnosis can be confirmed by looking for specific IgM antibodies in the fetal blood. The blood can also be analysed for abnormal liver functions and for thrombocytopenia.
Others
Infections like listeriosis can lead to miscarriage or neonatal meningitis. Parvovirus B-19 infections can cause severs anemia and hydrops fetalis resulting in fetal loss.
PHYSICAL AGENTS
Ionizing Radiations
Heavy doses of ionizing radiation can lead to microcephaly and eye defects. They can have mutagenic and carcinogenic effects. The most critical period is 2-5 weeks post conception. Irrespective of the dose ionizing radiations should be avoided in pregnancy.
Hyperthermia
Prolonged hyperthermia occuring in early pregnancy can cause microcephaly and microphthalmia in the fetus. Nerve migration defects are also reported. Hot baths and saunas should be avoided in first trimester.
Maternal illness
Maternal disease in pregnancy poses a two-fold problem. The effects could be due to the disease itself, or to the drugs administered for the disease. Improvements in neonatal and pediatric care have given an opportunity to individuals with genetic disorders to reach a reproductive age group. Thus clinicians caring for a pregnant women should not only be familiar with routinely seen medical disorders such as hypertension and diabetes or infectious diseases like HIV or syphilis but genetic diseases like cystic fibrosis.
Diabetes Mellitus
Incidence of birth defects in mothers with diabetes is increased two to three fold as compared with the population. Commonly known malformations are congenital heart disease, neural tube defects, sacral agenesis, and sirenomelia. Monitoring of blood glucose levels and glucose and glycosylated hemoglobin level in the mothers is recommended. Gestational diabetes does not increase the risk of malformations.
Epilepsy
Maternal epilepsy by itself does not pose a threat to pregnancy as regards congenital malformations. It may lead to a depletion in placental circulation during an attack. Anticonvulsant drugs are known to have teratogenic effects. Phenytoin has an increased risk for cleft lip and palate, and sodium valproate has an increased risk for anencephaly and spinabifida. A combination of drugs is more teratogenic. However, the risks of withholding drugs and of recurrence of seizures have to be weighed appropriately during care of the pregnant mother.
Phenylketonuria
Untreated maternal PKU leads to mental retardation in the child. In addition microcephaly and congenital heart defects are known. A low phenylalanine diet before and during pregnancy is necessary.
References
Purandarey, H. (2009). Essentials of Human Genetics. Second Edition. Jaypee Brothers Medical Publishers (P) Ltd.



|
|
|
|
دراسة يابانية لتقليل مخاطر أمراض المواليد منخفضي الوزن
|
|
|
|
|
|
|
اكتشاف أكبر مرجان في العالم قبالة سواحل جزر سليمان
|
|
|
|
|
|
|
اتحاد كليات الطب الملكية البريطانية يشيد بالمستوى العلمي لطلبة جامعة العميد وبيئتها التعليمية
|
|
|