
Thyroid gland
 المؤلف:
Kelly M. Harrell and Ronald Dudek
المؤلف:
Kelly M. Harrell and Ronald Dudek
 المصدر:
Lippincott Illustrated Reviews: Anatomy
المصدر:
Lippincott Illustrated Reviews: Anatomy
 الجزء والصفحة:
الجزء والصفحة:
 1-8-2021
1-8-2021
 3853
3853
Thyroid gland
The thyroid gland is a bilobar endocrine organ responsible for production of thyroid hormone and calcitonin. These products regulate rate of metabolism and calcium metabolism, respectively. The thyroid gland is located anteriorly in the muscular triangle just inferior to the thyroid cartilage. Its midline connection-isthmus-is located at approximately the second or third tracheal ring level. Deep to the visceral fascia, the thyroid has a separate fibrous capsule that further divides the gland with intraglandular septa (Fig. 1).
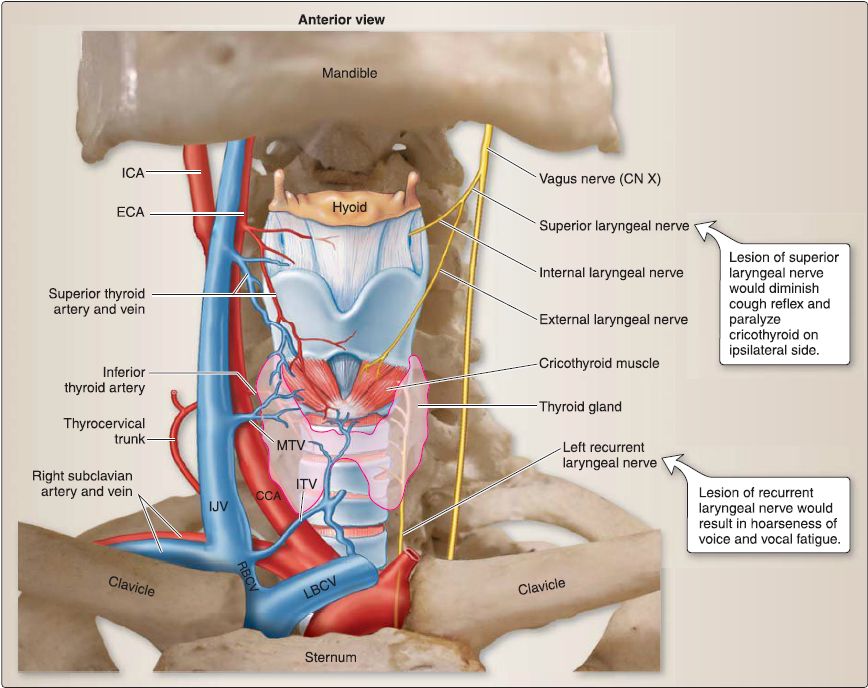
Figure 1: Viscera of the neck and associated structures. CCA = common carotid artery, CN = cranial nerve, ECA = external carotid artery, ICA = internal carotid artery, IJV = internal jugular vein, ITV= inferior thyroid vein, LBCV = left brachiocephalic vein, MTV = middle thyroid vein, RBCV = left brachiocephalic vein.
1. Vasculature: The thyroid gland receives blood supply from the
superior and inferior thyroid arteries, which arise from the external carotid and thyrocervical trunk, respectively. Bilaterally, these vessels pierce the visceral fascia (pretracheal) and anastomose within the gland to ensure adequate collateral circulation. Superior, middle, and inferior thyroid veins drain the thyroid gland.
Superior and middle thyroid veins are tributaries of the internal jugular vein, whereas the inferior thyroid vein drains directly into the brachiocephalic veins.
2. Lymphatics: Lymphatic drainage of the thyroid gland starts at associated lymph nodes, which include pretracheal, paratracheal, and prelaryngeal groups. Lymph then drains into deep cervical nodes.
3. Innervation: The thyroid gland receives autonomic innervation via postganglionic sympathetic fibers from the cervical sympathetic ganglia . These fibers distribute along the vasculature and function only to regulate vasoconstriction. Glandular function is regulated strictly by the pituitary gland.
4. Embryology: At week 4, the thyroid primordium, a small mass of endoderm, forms in the mid line of the floor of the pharynx near the foramen cecum of the developing tongue. The thyroid primordium migrates caudally down the midline, passing ventral to the hyoid bone and the laryngeal cartilages to its adult location. During this migration, the thyroid primordium remains connected to the tongue by the thyroglossal duct. By week 5, the thyroglossal duct is obliterated, leaving only a remnant called the foramen cecum (Fig. 2). The endoderm of the thyroid primordium eventually differentiates into the thyroid follicular cells. In addition, the neural crest cells within the ultimopharyngeal body (i.e., pharyngeal pouch 4) disperse throughout the thyroid gland and differentiate into the parafollicular cells (or C cells).

Figure 2: Embryology of the thyroid.
5. Histology: The normal adult thyroid gland is red brown in color and butterfly shaped with two bulky lateral lobes connected by a thin isthmus. Each lateral lobe is about 2 cm wide by 6 cm long by 2 cm thick. The normal adult thyroid gland weighs about 15-25 g.
[1] Thyroid follicle: The thyroid gland is surrounded by a connective tissue capsule that sends trabeculae into the interior of the gland to provide a delicate loose connective tissue stroma that surrounds the thyroid follicles. The functional unit of the thyroid gland is the thyroid follicle (Fig. 3). The thyroid follicle is a spherical structure that contains a gel-like substance called colloid that is composed mainly of iodinated thyroglobulin (660 kDa). Thyroglobulin is the inactive storage form of the thyroid hormones (triiodothyronine [T 3] and thyroxin [T 41). The wall of the thyroid follicle is formed by follicular cells and parafollicular cells.
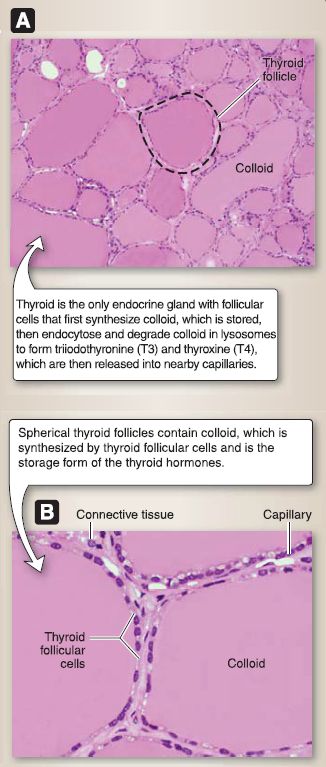
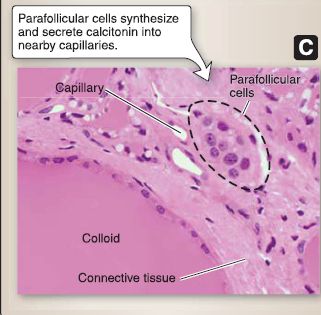
Figure 2: Thyroid histology. Thyroid follicles at a low (A) and higher (B) magnification. C, Parafollicular cells.
[2] Follicular cells: The follicular cell is a cuboidal-shaped cell in an inactive thyroid gland and columnar-shaped cell in an active thyroid gland. It has a round, basally located nucleus with one or more nucleoli. Follicular cells contain rough endoplasmic reticulum, polyribosomes, a Golgi complex, mitochondria, endocytotic vesicles, juxtaluminal zonula occludens (tight junctions), apical microvilli, lysosomes, and lipid droplets. They synthesize iodinated thyroglobulin and secrete T 3 and T 4, both of which are lysosomal degradation products of iodinated thyroglobulin.
[3] Parafollicular cell: The parafollicular cell is a spherical cell with a round, centrally located nucleus. It contains rough endoplasmic reticulum, polyribosomes, a Golgi complex, mitochondria, and numerous secretory granules. Parafollicular cells may lie within the basal lamina that surrounds thethyroid follicle or as a cluster of cells in the loose connective tissue between follicles. They synthesize and secrete calcitonin. Calcitonin lowers blood Ca2+ levels by acting directly on osteoclasts to decrease their bone resorption activity.
 الاكثر قراءة في علم التشريح
الاكثر قراءة في علم التشريح
 اخر الاخبار
اخر الاخبار
اخبار العتبة العباسية المقدسة


