


 النبات
النبات
 الحيوان
الحيوان
 الأحياء المجهرية
الأحياء المجهرية
 علم الأمراض
علم الأمراض
 التقانة الإحيائية
التقانة الإحيائية
 التقنية الحيوية المكروبية
التقنية الحيوية المكروبية
 التقنية الحياتية النانوية
التقنية الحياتية النانوية
 علم الأجنة
علم الأجنة
 الأحياء الجزيئي
الأحياء الجزيئي
 علم وظائف الأعضاء
علم وظائف الأعضاء
 الغدد
الغدد
 المضادات الحيوية
المضادات الحيوية|
Read More
Date: 30-7-2021
Date: 1-8-2021
Date: 9-7-2021
|
Oral Region
Structures of the oral region include those found in the oral cavity and the transitional region between the oral cavity and the oropharynx, including the teeth, tongue, gums, soft and hard palates, and palatine tonsils.
A. Oral cavity
The oral cavity (mouth) represents the beginning of the gastrointestinal tract (Fig. 1). Food is ingested into the oral cavity and prepared for digestion. The roof of the oral cavity is formed by the hard and soft palates, whereas the floor is formed by the tongue and associated mucous membrane. The mylohyoid and geniohyoid muscles lie
superficial to the mucosa and further support the floor of the mouth. Sensory innervation to the roof and floor of the oral cavity is mediated through branches of the maxillary and mandibular divisions of the trigeminal nerve {V2 and V3), respectively. The oral cavity receives blood supply from branches of the maxillary, facial, and lingual arteries. The oral cavity can be divided into the following two regions.
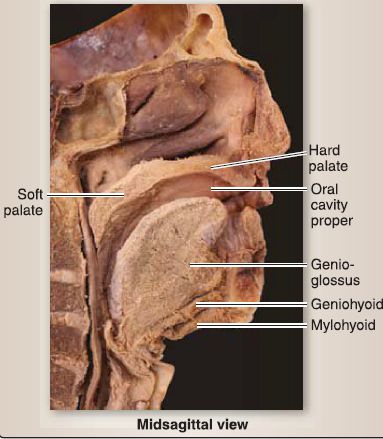
Figure 1: Oral cavity.
1. Oral vestibule: This is a Li-shaped interval between the lips/cheeks and teeth/gums. The parotid duct opens into this space opposite the upper second molar.
2. Oral cavity proper: This is the area between the arches of the teeth, containing the tongue, sublingual mucosa, frenulum, and submandibular gland ducts.
B. Palate
The formation of the adult palate occurs as a result of the embryologic development and fusion of the primary and secondary palates.
1. Embryology: During week 7, the intermaxillary segment forms when the two medial nasal prominences fuse together at the midline due to the growth of the maxillary prominences of pharyngeal arch 1 toward the midline .
a. Primary palate: The intermaxillary segment forms the philtrum of the lip, four incisor teeth, and the primary palate.
b. Secondary palate: The secondary palate forms from horizontal outgrowths of the maxillary prominences of pharyngeal arch 1 called the palatine shelves. Initially, the palatine shelves project downward on either side of the tongue but later attain a horizontal position and fuse along the palatine raphe to form the secondary palate.
c. Definitive palate: The primary and secondary palates fuse at the incisive foramen to form the definitive palate. Bone develops in both the primary palate and anterior part of the secondary palate. Bone does not develop in the posterior part of the secondary palate, which eventually forms the soft palate and uvula.
d. Nasal septum: The nasal septum develops from the frontonasal prominence and medial nasal prominences and grows down vertically from the roof of the primitive nasal chamber. The nasal septum eventually fuses with the definitive palate and divides the primitive nasal chamber into two nasal passages.
2. Anatomy: The hard and soft palates collectively form the roof of the oral cavity and the floor of the nasal cavity (Fig. 2).
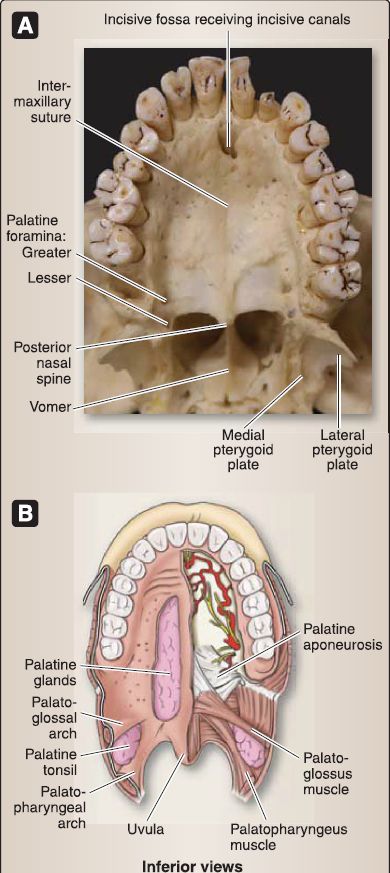
Figure 2: Palate. A, Hard palate. B, Soft palate.
a. Hard palate: Anteriorly, the hard palate represents two-thirds of the palate and is made up of the maxillae (palatine processes) and palatine {horizontal plate) bones, covered in a thick mucosa that contains palatine glands.
b. Soft palate: The soft palate makes up the posterior third of the palate and marks the transitional area between the oral cavity and the oropharynx superiorly. This mobile soft tissue partition arches posteroinferiorly in the midline as the uvula and receives support from a strong palatine aponeurosis.
c. Musculature: Muscles of the palate include the tensor veli palatini, levator veli palatini, musculus uvulae, palatoglossus, and palatopharyngeus. The palatoglossus and palatopharyngeus muscles form the palatine arches that contain palatine tonsils and mark the transition from the oral cavity to the oropharynx inferiorly.
[1] Tensor veli palatini: This muscle is innervated by CN V3 and functions to tense the soft palate and open the auditory tube during swallowing and yawning (think popping ears with changes in altitude).
[2] Levator veli palatini: This muscle is innervated by the vagus nerve (CN X) and functions to elevate the soft palate.
[3] Musculus uvulae: This muscle is innervated by CN X and functions to pull the uvula superiorly.
[4] Palatoglossus: This muscle is innervated by CN X and functions to depress the soft palate and elevate the tongue.
[5] Palatopharyngeus: This muscle is innervated by CN X and functions to tense the soft palate and move the pharyngeal walls during swallowing.
d. Innervation: Terminal branches of V2 and the maxillary artery reach the palate by way of one of three bony foramina-incisive canal/fossa, greater palatine foramen, and lesser palatine foramen. Nerves of the palate include the nasopalatine and greater
and lesser palatine branches of V 2• These nerves provide general sensation to the palate and also carry postganglionic autonomic fibers to the palatine glands. The mucosa overlying the region of the palatal arches and tonsils is primarily served by the glossopharyngeal nerve (CN IX). Stroking of this mucosa typically elicits the gag reflex and tests the integrity of CN IX. The greater and lesser palatine arteries supply the hard and soft palates, respectively.
C. Tongue and salivary glands
The body (oral part; anterior two-thirds) of the tongue fills the floor of the oral cavity, and the root (pharyngeal part; posterior third) of the tongue occupies the anterior portion of the oropharynx. The tongue is a strong, moveable organ composed of intrinsic musculature covered in a thick mucous membrane. The tongue functions in mastication, speech, taste, expression, and swallowing.
1. Embryology: Late in week 4, a number of swellings appear in the floor of the pharynx, which consist of mounds of mesoderm covered by endoderm (Fig. 3). These swellings are responsible for forming the oral part of the tongue (i.e., the anterior two-thirds of I]) the tongue), the pharyngeal part of the tongue (i.e., the posterior third of the tongue), and the tongue musculature.
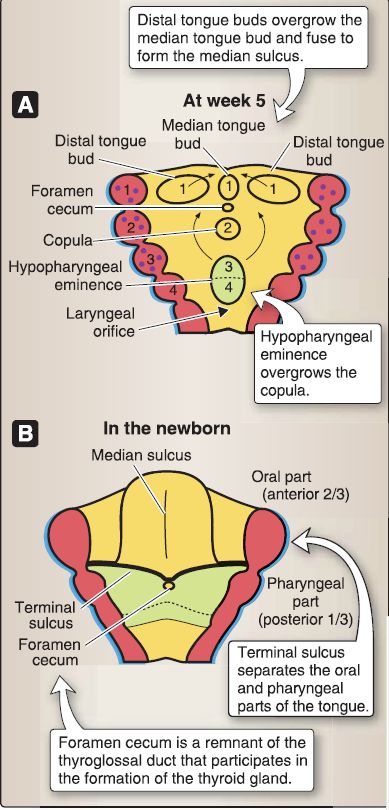
Figure 3: Development of the tongue (A and B).
a. Oral part: The oral part of the tongue forms from the median tongue bud and two distal tongue buds consisting of mounds of mesoderm covered by endoderm. The median tongue bud and two distal tongue buds develop in the floor of the pharynx due to a proliferation of mesoderm associated with pharyngeal arch 1. The distal tongue buds overgrow the median tongue bud and fuse in the midline, forming the median sulcus.
[1] Taste buds: The oral part of the tongue is characterized by filiform papillae (no taste buds), fungiform papillae (taste buds present), foliate papillae (taste buds present), and circumvallate papillae (taste buds present).
[2] General sensation: General sensation from the mucosa (derived from endoderm) of the oral part of the tongue is carried by the lingual branch of the trigeminal nerve (CN V).
[3] Taste sensation: Taste sensation from the mucosa (derived from endoderm) of the oral part of the tongue is carried by the chorda tympani branch of the facial nerve (CN VII). Special visceral afferent neurons convey taste sensation from the oral part of the tongue to the CNS. The cell bodies for these neurons lie in the geniculate ganglion. The peripheral processes run with the lingual nerve and chorda tympani nerve. The central processes enter the brainstem via the intermediate nerve and terminate in the rostral portion of the solitary nucleus.
b. Pharyngeal part: The pharyngeal part of the tongue forms from the copula and the hypopharyngeal eminence, which consist of mounds of mesoderm covered by endoderm. The copula develops in the floor of the pharynx due to a proliferation of mesoderm associated with pharyngeal arch 2. The hypopharyngeal eminence develops in the floor of the pharynx due to a proliferation of mesoderm associated with pharyngeal arches 3 and 4. The hypopharyngeal eminence (pharyngeal arches 3 and 4) overgrows the copula (pharyngeal arch 2), thereby eliminating any contribution of the copula (pharyngeal arch 2) in the formation of the definitive adult tongue.
[1] Tonsils: The line of fusion between the oral and pharyngeal parts of the tongue is indicated by the terminal sulcus. The pharyngeal part is characterized by the lingual tonsil, which forms along with the palatine tonsil and pharyngeal tonsil (adenoids) Waldeyer's ring.
[2] General and taste sensations: General and taste sensations from the mucosa (derived from endoderm) of the pharyngeal part of the tongue are carried primarily by the glossopharyngeal nerve (CN IX).
c. Musculature: The intrinsic muscles and most of the extrinsic muscles of the tongue are derived from myoblasts that migrate into the tongue region from occipital myotomes. The motor innervation to these muscles is supplied by the hypoglossal nerve (CN XII).
[1] Extrinsic muscle: The extrinsic muscle of the tongue that is the exception is the palatoglossus muscle, which is derived from mesoderm probably associated with pharyngeal arch 4 and is innervated by the pharyngeal plexus of nerves derived from the vagus nerve (CN X).
2. Histology: The tongue consists of a mucosa (stratified squamous epithelium and connective tissue), skeletal muscle, and seromucous glands (Fig. 4). The intrinsic skeletal muscle bundles are arranged in three separate planes (longitudinal, transverse, and vertical) at right angles to one another. The seromucous glands and their ducts are found interspersed between the skeletal muscle bundles.
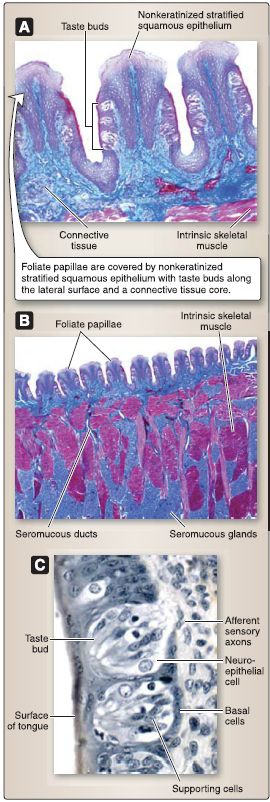
Figure 4: Tongue histology (A-C).
a. Mucosa: The ventral mucosa consists of nonkeratinized stratified squamous epithelium and connective tissue similar to the lining of the oral cavity. The dorsal mucosa is highly specialized, consisting of four types of papillae that consist of a keratinized stratified squamous epithelium and connective tissue.
[1] Filiform papillae: These are the most numerous and smallest of the four types of papillae. The filiform papillae cover the entire anterior two-thirds of the tongue. They contain no taste buds but instead help in chewing and mixing food.
[2] Fungiform papillae: These are less numerous and taller than filiform papillae. The fungiform papillae are found near the tip and sides of the tongue. They contain taste buds along their apical surface.
[3] Foliate papillae: These are found along the posterior lateral edge of the tongue as a series of parallel ridges. The foliate papillae are not well developed in humans: in young individuals, foliate papillae can be observed, but, in older individuals, they may not be. The foliate papillae contain taste buds along their lateral surface.
[4] Circumvallate papillae: These are the largest of the four types of papillae. The circumvallate papillae (10-14 in number) are found in a single row just anterior to the sulcus terminalis of the tongue. They are surrounded by a deep groove into which serous glands (glands of von Ebner) open. The circumvallate papillae contain taste buds along their lateral surface.
b. Taste buds: The taste buds are oval, light-staining structures found within the nonkeratinized stratified squamous epithelium that sense the contents of the oral cavity through the taste pore. They consist of the following cells.
[1] Neuroepithelial cells: The neurosensory cells have a large, round, light-staining nucleus and apical microvilli that extend into the taste pore. The neurosecretory cells synapse with afferent sensory nerve axons at their basal surface.
[2] Supporting cells: The supporting cells have a narrow, flat, dark-staining nucleus and apical microvilli that extend into the taste pore.
[3] Basal cells: The basal cells are small cells located at the base of the taste bud and serve as stem cells.
3. Anatomy: The tongue can move and change shape through coordinated movements of intrinsic and extrinsic muscles.
a. Intrinsic muscles: These are contained within the tongue and have no bony attachments. Intrinsic muscles are arranged in longitudinal, transverse, and vertical bands. These muscles primarily act to alter the shape of the tongue. All intrinsic muscles are innervated by the hypoglossal nerve (CN XII).
b. Extrinsic muscles: Extrinsic tongue muscles arise from bone and insert into various parts of the tongue (Fig. 5). These muscles primarily act to alter the position of the tongue. All extrinsic tongue muscles, with the exception of the palatoglossus, are innervated by the hypoglossal nerve (CN XII). The palatoglossus is innervated by the vagus nerve (CN X). Extrinsic tongue muscles include the following.

Figure 5: Intrinsic and extrinsic tongue muscles. A, Cadaveric specimen. B, Primary
extrinsic tongue muscles (palatoglossus not shown).
[1] Genioglossus: Originating from the mental spine of the mandible, this muscle's functions include tongue depression,protrusion, and lateral movements.
[2] Hyoglossus: Originating from the hyoid bone, this muscle functions primarily to depress the tongue.
[3] Styloglossus: Originating from the styloid process, this muscle functions primarily to retract the tongue.
[4] Palatoglossus: Originating from the palatine aponeurosis, this muscle functions to elevate the posterior tongue toward the soft palate.
c. General sensation: General sensation to the anterior two thirds and posterior third is mediated by the lingual nerve (CN V3) and the glossopharyngeal nerve (CN IX), respectively (Fig. 6).

Figure 6: Tongue innervation and vasculature.
d. Taste sensation: Taste to the anterior two thirds and posterior third is mediated by the chorda tympani nerve (CN VII) and glossopharyngeal nerve, respectively (see Fig. 8.53). The vagus nerve (CN X) also mediates a small area of taste on the root of the tongue adjacent to the epiglottis.
e. Vasculature: Vasculature of the tongue includes branches of the lingual artery, which arises from the external carotid artery (see Fig. 6). Passing deep to the hyoglossus muscle to reach the tongue, the lingual artery gives off dorsal, deep, and sublingual branches. Dorsal and deep lingual veins drain the tongue. Lymphatic drainage occurs by way of the superior and inferior deep cervical lymph nodes for the posterior third and anterior two thirds, respectively. The lateral surfaces of the tongue are drained into the submandibular lymph nodes.
f. Organization: The arrangement of structures associated with the tongue is such that the lingual nerve with the submandibular ganglion and the hypoglossal nerve passes lateral to the hyoglossus muscle to reach the tongue mucosa and musculature,
respectively. The lingual artery passes medial to the hyoglossus
muscle to reach the tongue.
4. Salivary glands: Salivary glands produce and secrete saliva into the oral vestibule and cavity (Fig. 7). These include the parotid, submandibular, and sublingual glands, in addition to the smaller mucous glands of the palate.
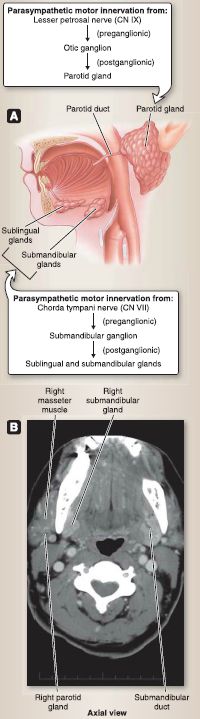
Figure 7: Salivary glands. A, Glands and associated structures. B, CT scan showing parotid and submandibular glands. C, Axial CT image. CT= computed tomography.
a. Parotid gland: The parotid gland sits in the parotid bed situated between the mandibular ramus and mastoid process, anterior to the external ear and inferior to the zygomatic arch. The largest of the salivary glands in the head, it is encased in a thick connective tissue sheath-the parotid sheath-and is traversed by several important structures of the head and face. In particular, the facial nerve divides the gland into superficial and deep lobes. The retromandibular vein and external carotid artery pass through the deep lobe.
[1] Parotid duct: The parotid duct (Stensen's duct) extends anteriorly across the masseter, often running with the buccal branch of the facial nerve (CN VII), and pierces the buccinator muscle to enter the oral cavity at the level of the second maxillary molar tooth.
[2] Innervation: Sensory innervation to the parotid sheath and overly skin is mediated by the great auricular nerve (C2-C3) of the cervical plexus. Parasympathetic autonomic innervation (general visceral efferent [GVE]) is provided by a branch of the glossopharyngeal nerve (CN IX)-lesser petrosal nerve-which synapses in the otic ganglion in the infratemporal fossa, and postganglionic fibers ride on the auriculotemporal nerve (CN V3) to reach the parotid gland. Postganglionic sympathetic fibers from the superior cervical ganglion reach the parotid gland through the external carotid plexus.
b. Submandibular gland: The submandibular gland is the next largest gland. It can be divided into superficial and deep portions, with the superficial portion occupying part of the submandibular triangle in the neck and the deep portion lying medial to the body of the mandible. The submandibular duct arises from the deep portion and travels anteriorly before opening into the floor of the mouth on either side of the frenulum of the tongue at the sublingual papillae.
c. Sublingual glands: The sublingual glands are the smallest and deepest of the salivary glands. They lie deep to the mucosa of the oral cavity floor and join bilaterally to form a U-shaped elevation beneath the mucosal lining. A series of small ducts extend superiorly from the glands to empty into the floor of the mouth.
d. Innervation: The submandibular and sublingual glands receive parasympathetic autonomic (GVE) innervation from postganglionic fibers that arise from the submandibular ganglion that is suspended from the lingual nerve (CN V3). Preganglionic fibers from the chorda tympani nerve (CN VII) synapse in the submandibular ganglion to complete this autonomic chain.
5. Histology: Figure 8shows the histology of the salivary glands. a. Parotid gland: The parotid gland is a serous gland arranged as a compound tubuloacinar gland. The parotid gland is surrounded by a connective tissue capsule that divides the gland into lobes and lobules.
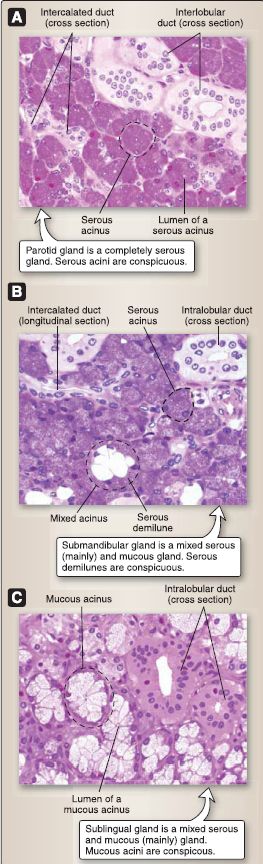
Figure 7: Salivary glands histology. A, Parotid gland. B, Submandibular gland. C, Sublingual gland.
[1] Serous cells: These are pyramidal-shaped cells with a broad basal surface abutting the connective tissue and a narrow apical surface abutting the lumen of the acinus. Serous cells have a round, basally located nucleus. They are protein-secreting cells (they also secrete H2O and ions)with basophilia located at the basal cytoplasm representing the rough endoplasmic reticulum.
[2] Duct system: The duct system of the parotid gland consists of intercalated, intralobular (striated), and interlobular ducts and the main excretory duct. The intercalated duct is lined by a simple low cuboidal epithelium and receives secretions from the serous acinus directly. The intralobular (striated) duct is lined by a simple columnar epithelium characterized by basal infoldings that modify the initial secretion from the acini by altering the concentration of various electrolytes.
The interlobular duct and excretory ducts are lined by a pseudostratified, stratified cuboidal, or stratified columnar epithelium and are located within connective tissue septae from the capsule.
b. Submandibular gland: The submandibular gland is a mixed serous (mainly) gland and mucous gland arranged as a compound tubuloacinar gland. It is surrounded by a connective tissue capsule that divides the gland into lobes and lobules. Secretory acini that contain both serous and mucous cells are called "mixed acini."
[1] Serous cells: These are the same as those of the parotid gland as described above. They are located at the periphery of mixed acini and are called serous demilunes because they appear as a half-moon shape.
[2] Mucous cells: These are pyramidal-shaped cells with fairly distinct basal, lateral, and apical margins. Mucous cells have a flat, oval-shaped nucleus. They are glycoprotein-secreting cells with basophilia located at the basal cytoplasm representing the rough endoplasmic reticulum and apical mucous droplets that appear as clear vacuoles because mucus is extracted during histologic processing.
[3] Duct system: The duct system of the submandibular gland is the same as that of the parotid gland as described above.
c. Sublingual gland: The sublingual gland is a mixed serous gland and mucous (mainly) gland arranged as a compound tubuloacinar gland. It is surrounded by a connective tissue capsule that divides the gland into lobes and lobules.
[1] Serous and mucous cells: These are the same as those described above; however, serous demilunes are not prominent in the sublingual gland.
[2] Duct system: The duct system of the sublingual gland consists of intercalated ducts, intralobular ducts, interlobular ducts, and the main excretory duct. The intercalated duct is lined by a simple low cuboidal epithelium and receives secretions from the acinus directly. The intercalated ducts in the sublingual gland are short and, therefore, difficult to observe. The intralobular duct is lined by a simple columnar epithelium and is not characterized by basal infoldings.
The interlobular duct and excretory ducts are lined by a pseudostratified, stratified cuboidal, or stratified columnar epithelium and are located within connective tissue septae from the capsule.
6. Teeth and gums: In the adult, 32 teeth are typically housed inthe upper and lower jaws (Fig. 8). These permanent teeth include four incisors, two canines, four premolars, and six molars in each jaw.
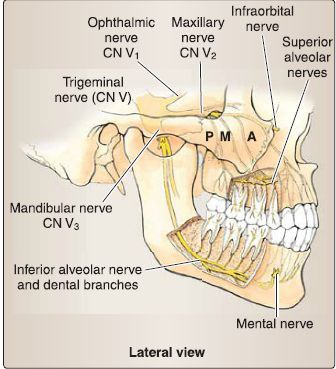
Figure 8: Teeth and gum innervations: trigeminal nerve, mandibular ,Y2) and maxillary ,Y3) divisions. A = anterior, M = middle, P = Posterior.
a. Anatomy: Teeth have three main parts-crown, neck, and root. The root is anchored tightly into dental alveoli by a periodontal membrane. The neck represents the transition zone between the root and the crown. The crown extends into the oral cavity from the gingiva (gums). Enamel covers the surface of the crown, whereas dentine forms the majority of the core of each tooth.
b. Innervation: The teeth and gums associated with the maxilla receive sensory innervation from the posterior, middle, and anterior superior alveolar branches from the maxillary division of the trigeminal nerve (CN V2). The teeth associated with the mandible receive sensory innervation from dental branches of the inferior alveolar nerve, a branch of the mandibular division of the trigeminal nerve (CN V3). The buccal and lingual gums of the mandible receive sensory innervation from the buccal and lingual nerves (CN V3), whereas the palatal gingiva receives sensory innervation from the nasopalatine, greater palatine, and lesser palatine nerves (CN V2).
c. Arterial supply: Blood supply to the upper and lower jaw structures includes branches of the maxillary artery, including the posterior superior alveolar, inferior alveolar, buccal, greater and lesser palatine, and sphenopalatine arteries.



|
|
|
|
تفوقت في الاختبار على الجميع.. فاكهة "خارقة" في عالم التغذية
|
|
|
|
|
|
|
أمين عام أوبك: النفط الخام والغاز الطبيعي "هبة من الله"
|
|
|
|
|
|
|
قسم شؤون المعارف ينظم دورة عن آليات عمل الفهارس الفنية للموسوعات والكتب لملاكاته
|
|
|