
Abdominal Viscera Innervation
 المؤلف:
Kelly M. Harrell and Ronald Dudek
المؤلف:
Kelly M. Harrell and Ronald Dudek
 المصدر:
Lippincott Illustrated Reviews: Anatomy
المصدر:
Lippincott Illustrated Reviews: Anatomy
 الجزء والصفحة:
الجزء والصفحة:
 16-7-2021
16-7-2021
 2397
2397
Abdominal Viscera Innervation
Innervation of the abdominal viscera occurs through an intricate network of autonomic ganglia and plexuses that are organized principally along the anterior surface of the abdominal aorta and along associated paired and unpaired aortic branches (Fig. 1). These autonomic structures collectively constitute the aortic plexus, which is described as prevertebral (preaortic), as opposed to the paravertebral sympathetic trunks that run on either side of the vertebral bodies. Sympathetic and parasympathetic (general visceral efferent [GVE]) components differ significantly in their origin and slightly in their overall pattern once in the abdominal cavity. In general, both fiber types travel into the abdominal cavity as preganglionic fibers before synapsing on either prevertebral ganglia (sympathetic) or on ganglia in the walls of viscera (parasympathetic).
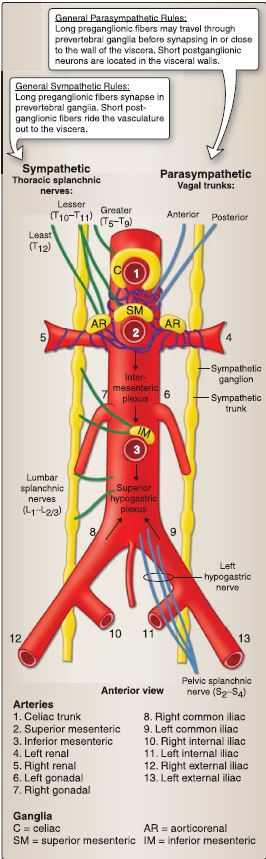
Figure 1: General organization and contents of aortic plexus.
A. Aortic plexus
The aortic plexus spans between vertebral levels T12 to L3, primarily on the anterior surface of the abdominal aorta. Sympathetic ganglia and mixed (sympathetic and parasympathetic) autonomic fibers that make up subsidiary plexuses are named by the arteries they surround. Named mixed plexuses include celiac, renal, intermesenteric, inferior mesenteric, and superior hypogastric. Named sympathetic ganglia associated with these plexuses include celiac, superior mesenteric, aorticorenal, and inferior mesenteric. These ganglia contain postganglionic sympathetic neurons. Postganglionic parasympathetic neurons are primarily located in visceral walls. Autonomic fibers from these plexuses travel on vasculature to reach abdominal viscera. Although the pattern of preganglionic sympathetic fiber distribution to prevertebral ganglia is well established, some fibers will bypass adjacent ganglia and travel through other plexuses to reach more lateral or inferior ganglia.
B. General visceral efferent innervation, sympathetic
Sympathetic (GVE) innervation of abdominal viscera occurs through preganglionic thoracic (greater, lesser, and least) and lumbar splanchnic nerves. Typically, these preganglionic sympathetic fibers travel to prevertebral (preaortic) plexuses and synapse in associated ganglia.
1. Thoracic splanchnic nerves: These nerves have cell bodies that originate in the lateral horn (intermediolateral cell column) of the thoracic spinal cord (T5-Td).
a. Greater splanchnic nerve: This nerve originates at T5-T9 and travels to synapse on postganglionic cell bodies in the celiac ganglion. These fibers distribute primarily on branches of the celiac trunk to reach viscera. In general, these postganglionic fibers distribute to foregut structures in the abdomen.
b. Lesser splanchnic nerve: This nerve originates at T10-T11 and travels to synapse on postganglionic cell bodies in the celiac and superior mesenteric ganglia. These fibers may distribute through celiac, superior mesenteric, and renal plexuses to reach viscera. In general, these postganglionic fibers distribute to midgut structures and the kidneys.
c. Least splanchnic nerve: This nerve originates at T12 and travels to synapse on postganglionic cell bodies in the aorticorenal ganglia. These fibers distribute through superior renal plexuses to reach viscera.
2. Lumbar splanchnic nerves: These nerves have cell bodies that originate in the lateral horn (intermediolateral cell column) of the lumbar spinal cord (L1-L213).
a. Upper lumbar splanchnic nerves: These originate at L1-L2 and travel to synapse primarily in the inferior mesenteric ganglion. Postganglionic fibers travel through the intermesenteric plexus and distribute along branches of the inferior mesenteric artery to reach viscera. In general, these postganglionic fibers distribute to hindgut structures.
b. Lower lumbar splanchnic nerves: These originate at L1-L2 but exit the sympathetic trunk at L3-L4 levels. These nerves are not technically part of the aortic plexus. They feed into the superior hypogastric plexus, which provides a thruway for sympathetic fibers to reach pelvic viscera.
C. General visceral efferent innervation, parasympathetic
Parasympathetic (GVE) innervation of abdominal viscera occurs through preganglionic vagus nerves (cranial nerve [CN] X) and pelvic splanchnic nerves (S2-S4). Typically, these preganglionic parasympathetic fibers travel through prevertebral (preaortic) plexuses and synapse in the walls of abdominal viscera.
1. Vagus nerve: At the distal end of the esophagus, vagal fibers from the esophageal plexus converge to form left and right vagus nerves. With the rotation of the stomach, these nerves assume a more anterior and posterior position, respectively. At this point,
they are renamed anterior and posterior vagal trunks. These preganglionic fibers will bypass prevertebral ganglia and travel within the periarterial plexuses to reach the walls of the viscera. Vagal innervation covers foregut and midgut structures before
terminating at the distal third of the transverse colon.
2. Pelvic splanchnic nerves: Originating in the gray matter of spinal cord levels S2 , S3 , and S4, these preganglionic parasympathetic fibers exit the spinal nerve as these levels join the inferior hypogastric plexus, travel through the hypogastric nerves to the superior hypogastric plexus, and distribute along periarterial plexuses associated with hindgut structures (inferior mesenteric artery distribution).
D. General visceral afferent innervation
Afferent pain fibers (general visceral afferent [GVA]) from abdominal viscera up to the midpoint of the sigmoid colon travel back to the sympathetic preganglionic origin. For example, visceral pain from the stomach will travel back to T6-T9 spinal cord levels, which represent a portion of the greater splanchnic nerve. Due to the overlap with somatic afferents at these levels, visceral pain can be referred to somatic representations of involved levels-T6-T9 dermatomes. Pain from viscera located inferior to the midpoint of the sigmoid colon, as well as subconscious reflex sensations
throughout the abdominal viscera, travel back along the path of the pelvic splanchnic nerves (origin: S2-S4).
 الاكثر قراءة في علم التشريح
الاكثر قراءة في علم التشريح
 اخر الاخبار
اخر الاخبار
اخبار العتبة العباسية المقدسة


