
 النبات
النبات
 الحيوان
الحيوان
 الأحياء المجهرية
الأحياء المجهرية
 علم الأمراض
علم الأمراض
 التقانة الإحيائية
التقانة الإحيائية
 التقنية الحيوية المكروبية
التقنية الحيوية المكروبية
 التقنية الحياتية النانوية
التقنية الحياتية النانوية
 علم الأجنة
علم الأجنة
 الأحياء الجزيئي
الأحياء الجزيئي
 علم وظائف الأعضاء
علم وظائف الأعضاء
 الغدد
الغدد
 المضادات الحيوية
المضادات الحيوية|
Read More
Date: 7-3-2016
Date: 18-3-2016
Date: 2024-12-18
|
Actinomyces
Actinomycetes are part of the normal mucosal flora. These are Gram-positive rods that often occur in the form of branched filaments in young cultures. Conglomerates of microcolonies in pus form so-called sulfur granules. Actinomycetes are obligate anaerobes. The pathogens enter body tissues through mucosa defects. Monoinfections are rare, the most frequent case being actinomycetes-dominated endogenous polyinfections. Cervicofacial
actinomycosis, caused by oral cavity colonizer A. israelii, is the most frequent form of actinomycosis. Treatment includes surgical procedures and antibiosis with aminopenicillins.
The group of Gram-positive, irregular (pleomorphic), nonsporing rod bacteria includes many different genera that are normal components of the skin and mucosal flora (Table 4.3, p. 261). Pathogens in this group cause two characteristic diseases: diphtheria, caused by Corynebacterium diphtheriae and actinomycosis, caused mainly by Actinomyces israelii.
Actinomycetes are Gram-positive bacteria that tend to grow in the form of branched filaments. The resulting mycelial masses are, however, not observed in older cultures, which strongly resemble those of corynebacteria in their morphology.
Occurrence. Actinomycetes are part of the normal mucosal flora in humans and animals. They colonize mainly the oral cavity, and an actinomycosis infection is therefore always endogenous. Ninety percent of actinomycetes infections in humans are caused by A. israelii, with far fewer cases caused by A. naeslundii and other species.
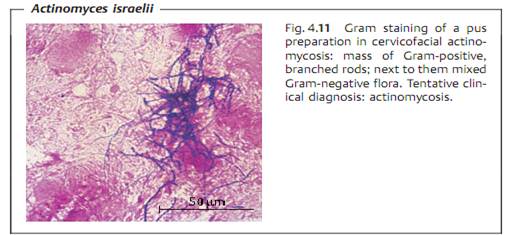
Morphology and culture. Actinomycetes are Gram-positive, pleomorphic rod bacteria that sometimes also show genuine branching (Fig. 4.11). The yellowish sulfur granules, measuring 1-2 mm, can be observed macroscopically in actinomycetes pus. These particles are conglomerates of small Actinomyces colonies surrounded by a wall of leukocytes. Mycelial filaments extend radially from the colonies (actinium = Greek for ray like). Culturing the organism requires enriched mediums and an anaerobic milieu containing 5-10% CO2. Mycelial microcolonies form only during the first days. Whitish macrocolonies, often with a rough surface, begin to appear after two weeks.
Pathogenesis and clinical picture. The pathogens breach mucosa (perhaps normal dermis as well) and are able to establish themselves in tissue in the presence of a low redox potential. The factors responsible for these conditions include poor blood perfusion and, above all, contributing bacterial
pathogens. Genuine actinomycoses are actually always polymicrobial. The mixed flora found includes mainly the anaerobes of the oral cavity. Actino-bacillus actinomycetemcomitans is frequently isolated along with various species of Bacteroidaceae. Facultative anaerobes such as staphylococci, streptococci, and Enterobacteriaceae are, however, also found among the contributing flora.
- Cervicofacial actinomycosis. This is the most frequent form of actinomy- cetes infection (>90%). The abscesses are hard and tumorlike at first, then they necrotize. They may also break through to the dermal surface to create fistulae.
- Thoracic actinomycosis. This rare form results from aspiration of saliva; sometimes this type also develops from an actinomycosis in the throat or hematogenous spread.
- Abdominal actinomycosis. This type results from injuries to the intestine or female genitals.
- Genital actinomycosis. May result from use of intrauterine contraceptive devices.
- Canaliculitis. An inflammation of the lacrimal canaliculi caused by any of several Actinomyces species.
- Caries. The Actinomyces species involved in caries development are A. vis- cosus, A. naeslundii, and A. odontolyticus . A possible contribution to periodontitis is also under discussion.
Diagnosis involves identification of the pathogen by microscopy and culturing in pus, fistula secretion, granulation tissue, or bronchial secretion. The samples must not be contaminated with other patient flora, in particular from the oral cavity and must be transported to the laboratory in special anaerobe containers. Microscopic detection of branched rods suffices for a tentative diagnosis. Detection of mycelial microcolonies on enriched nutrient mediums after one to two weeks further consolidates this diagnosis. Final identification by means of direct immunofluorescence, cell wall analysis, and metabolic analysis requires several weeks.
Therapy. Treatment includes both surgical and antibiotic measures. The antibiotic of choice is an aminopenicillin. Antibiosis that also covers the contributing bacterial pathogens is important.
Epidemiology and prevention. Actinomycoses occur sporadically worldwide. Average morbidity (incidence) levels are between 2.5 and five cases per 100 000 inhabitants per year. Men are infected twice as often as women. Prophylactic considerations are irrelevant due to the endogenous nature of actinomycetes infections.
Other Gram-Positive Rod Bacteria
Table 4.3 lists bacteria that are rarely involved in infections and normally infect only persons with defective immune defenses. Recent years have seen considerable changes in their classification and nomenclature-still an ongoing process. Many of these bacteria are part of the normal dermal and mucosal flora. They are frequently found in sampled materials as contaminants, but also occasionally cause infections. Some of these bacteria are designated by collective terms such as “diphtheroid rods” or “coryneform bacteria.”




|
|
|
|
التوتر والسرطان.. علماء يحذرون من "صلة خطيرة"
|
|
|
|
|
|
|
مرآة السيارة: مدى دقة عكسها للصورة الصحيحة
|
|
|
|
|
|
|
نحو شراكة وطنية متكاملة.. الأمين العام للعتبة الحسينية يبحث مع وكيل وزارة الخارجية آفاق التعاون المؤسسي
|
|
|