
 النبات
النبات
 الحيوان
الحيوان
 الأحياء المجهرية
الأحياء المجهرية
 علم الأمراض
علم الأمراض
 التقانة الإحيائية
التقانة الإحيائية
 التقنية الحيوية المكروبية
التقنية الحيوية المكروبية
 التقنية الحياتية النانوية
التقنية الحياتية النانوية
 علم الأجنة
علم الأجنة
 الأحياء الجزيئي
الأحياء الجزيئي
 علم وظائف الأعضاء
علم وظائف الأعضاء
 الغدد
الغدد
 المضادات الحيوية
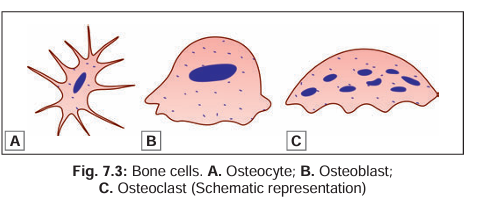
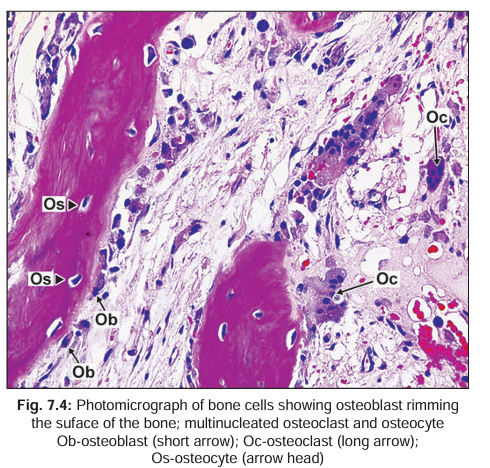
المضادات الحيويةLike cartilage, bone is a modified connective tissue. It consists of bone cells or osteocytes (Fig. 7.3) that are widely separated from one another by a considerable amount of inter cellular sub stance. The latter con sists of a homogeneous ground substance or matrix in which collagen fibres and mineral salts (mainly calcium and phosphorus) are deposited. In addition to mature bone cells (osteocytes) two additional types of cells are seen in developing bone. These are bone producing cells or osteo blasts, and bone removing cells or osteoclasts (Figs 7.3 and 7.4). Other cells present include osteoprogenitor cells from which osteoblasts and osteocytes are derived; cells lining the surfaces of bone; cells belonging to periosteum; and cells of blood vessels and nerves which invade bone from outside.
osteoprogenitor cells
These are stem cells of mesenchymal origin that can proliferate and convert themselves into osteoblasts whenever there is need for bone formation. They resemble fibroblasts in appearance. In the fetus such cells are numerous at sites where bone formation is to take place. In the adult, osteoprogenitor cells are present over bone surfaces (on both the periosteal and endosteal aspects).
Osteoblasts
These are bone forming cells derived from osteoprogenitor cells. They are found lining growing surfaces of bone, sometimes giving an epithelium-like appearance. However, on closer examination it is seen that the cells are of varied shapes (oval, triangular, cuboidal, etc.) and that there are numerous gaps between adjacent cells. The nucleus of an osteoblast is ovoid and euchromatic. The cytoplasm is basophilic because of the presence of abundant rough endoplasmic reticulum. This, and the presence of a well developed Golgi complex, signifies that the cell is engaged in considerable synthetic activity. Numerous slender cytoplasmic processes radiate from each cell and come into contact with similar processes of neighbouring cells.Osteoblasts are responsible for laying down the organic matrix of bone including the collagen fibres. They are also responsible for calcification of the matrix. Alkaline phosphatase present in the cell membranes of osteoblasts plays an important role in this function. Osteoblasts are believed to shed off matrix vesicles that possibly serve as points around which formation of hydroxyapatite crystals takes place. Osteoblasts may indirectly influence the resorption of bone by inhibiting or stimulating the activity of osteoclasts.
osteocytes
These are the cells of mature bone. They lie in the lacunae of bone, and represent osteoblasts that have become ‘imprisoned’ in the matrix during bone formation. Delicate cytoplasmic processes arising from osteocytes establish contacts with other osteocytes and with bone lining cells present on the surface of bone. In contrast to osteoblasts, osteocytes have eosinophilic or lightly basophilic cytoplasm. This is to be correlated with T he fact that these cells have negligible secretory activity T he presence of only a small amount of endoplasmic reticulum in the cytoplasm. Osteocytes are present in greatest numbers in young bone, the number gradually decreasing with age. Functions T he functions attributed to osteocytes are: T hey probably maintain the integrity of the lacunae and canaliculi, and thus keep open the channels for diffusion of nutrition through bone T hey play a role in removal or deposition of matrix and of calcium when required. osteoclasts These are bone removing cells. They are found in relation to surfaces where bone removal is taking place (Bone removal is essential for maintaining the proper shape of growing bone). At such locations the cells occupy pits called resorption bays or lacunae of Howship. Osteoclasts are very large cells (20 to 100 µm or even more in diameter). They have numerous nuclei: up to 20 or more. The cytoplasm shows numerous mitochondria and lysosomes containing acid phosphatase. At sites of bone resorption the surface of an osteoclast shows many folds that are described as a ruffled membrane. Removal of bone by osteoclasts involves demineralisation and removal of matrix. Bone removal can be stimulated by factors secreted by osteoblasts, by macrophages, or by lymphocytes. It is also stimulated by the parathyroid hormone. Recent studies have shown that osteoclasts are derived from monocytes of blood. It is not certain whether osteoclasts are formed by fusion of several monocytes, or by repeated division of the nucleus, without division of cytoplasm.
Bone lining Cells
These cells form a continuous epithelium-like layer on bony surfaces where active bone deposition or removal is not taking place. The cells are flattened. They are present on the periosteal surface as well as the endosteal surface. They also line spaces and canals within bone. It is possible that these cells can change to osteoblasts when bone formation is called for (In other words many of them are osteoprogenitor cells).
organic and inorganic Constituents of Bone matrix
The ground substance (or matrix) of bone consists of an organic matrix in which mineral salts are deposited.
The Organic Matrix
T his consists of a ground substance in which collagen fibres are embedded. The ground substance consists of glycosaminoglycans, proteoglycans and water. Two special glycoproteins osteonectin and osteocalcin are present in large quantity. They bind readily to calcium ions and, therefore, play a role in mineralisation of bone. Various other substances including chondroitin sulphates, phospholipids and phosphoproteins are also present. T he collagen fibres are similar to those in connective tissue (Type I collagen) (They are sometimes referred to as osteoid collagen). The fibres are usually arranged in layers, the fibres within a layer running parallel to one another. Collagen fibres of bone are synthesised by osteoblasts. T he matrix of bone shows greater density than elsewhere immediately around the lacunae, forming capsules around them, similar to those around chondrocytes in cartilage. The term osteoid is applied to the mixture of organic ground substance and collagen fibres (before it is mineralised).
The Inorganic Ions
The ions present are predominantly calcium and phosphorus (or phosphate). Magnesium, carbonate, hydroxyl, chloride, fluoride, citrate, sodium and potassium are also present in significant amounts. Most of the calcium, phosphate and hydroxyl ions are in the form of needle shaped crystals that are given the name hydroxyapatite (Ca10 [PO4 ]6 [OH]2 ). Hydroxyapatite crystals lie parallel to collagen fibres and contribute to the lamellar appearance of bone. Some amorphous calcium phosphate is also present. About 65% of the dry weight of bone is accounted for by inorganic salts, and 35% by organic ground substance and collagen fibres. (Note that these percentages are for dry weight of bone. In living bone about 20% of its weight is made up by water). About 85% of the total salts present in bone are in the form of calcium phosphate; and about 10% in the form of calcium carbonate. Ninety seven percent of total calcium in the body is located in bone.
T he calcium salts present in bone are not ‘fixed’ . There is considerable interchange between calcium stored in bone and that in circulation. When calcium level in blood rises calcium is deposited in bone; and when the level of calcium in blood falls calcium is withdrawn from bone to bring blood levels back to normal. These exchanges take place under the influence of hormones (parathormone produced by the parathyroid glands, and calcitonin produced by the thyroid gland).



|
|
|
|
يجب مراقبتها بحذر.. علامة في القدم تشير إلى مشاكل خطيرة
|
|
|
|
|
|
|
العلماء يحلون لغز بركان أدى إلى تجمد الأرض قبل 200 عام
|
|
|
|
|
|
|
رئيس جلسة العلوم الهندسية: بحوث مؤتمر جامعة الكفيل تقدم حلولًا عملية قابلة للتطبيق
|
|
|