النبات

مواضيع عامة في علم النبات

الجذور - السيقان - الأوراق

النباتات الوعائية واللاوعائية

البذور (مغطاة البذور - عاريات البذور)

الطحالب

النباتات الطبية


الحيوان

مواضيع عامة في علم الحيوان

علم التشريح

التنوع الإحيائي

البايلوجيا الخلوية


الأحياء المجهرية

البكتيريا

الفطريات

الطفيليات

الفايروسات


علم الأمراض

الاورام

الامراض الوراثية

الامراض المناعية

الامراض المدارية

اضطرابات الدورة الدموية

مواضيع عامة في علم الامراض

الحشرات


التقانة الإحيائية

مواضيع عامة في التقانة الإحيائية


التقنية الحيوية المكروبية

التقنية الحيوية والميكروبات

الفعاليات الحيوية

وراثة الاحياء المجهرية

تصنيف الاحياء المجهرية

الاحياء المجهرية في الطبيعة

أيض الاجهاد

التقنية الحيوية والبيئة

التقنية الحيوية والطب

التقنية الحيوية والزراعة

التقنية الحيوية والصناعة

التقنية الحيوية والطاقة

البحار والطحالب الصغيرة

عزل البروتين

هندسة الجينات


التقنية الحياتية النانوية

مفاهيم التقنية الحيوية النانوية

التراكيب النانوية والمجاهر المستخدمة في رؤيتها

تصنيع وتخليق المواد النانوية

تطبيقات التقنية النانوية والحيوية النانوية

الرقائق والمتحسسات الحيوية

المصفوفات المجهرية وحاسوب الدنا

اللقاحات

البيئة والتلوث


علم الأجنة

اعضاء التكاثر وتشكل الاعراس

الاخصاب

التشطر

العصيبة وتشكل الجسيدات

تشكل اللواحق الجنينية

تكون المعيدة وظهور الطبقات الجنينية

مقدمة لعلم الاجنة


الأحياء الجزيئي

مواضيع عامة في الاحياء الجزيئي


علم وظائف الأعضاء


الغدد

مواضيع عامة في الغدد

الغدد الصم و هرموناتها

الجسم تحت السريري

الغدة النخامية

الغدة الكظرية

الغدة التناسلية

الغدة الدرقية والجار الدرقية

الغدة البنكرياسية

الغدة الصنوبرية

مواضيع عامة في علم وظائف الاعضاء

الخلية الحيوانية

الجهاز العصبي

أعضاء الحس

الجهاز العضلي

السوائل الجسمية

الجهاز الدوري والليمف

الجهاز التنفسي

الجهاز الهضمي

الجهاز البولي


المضادات الميكروبية

مواضيع عامة في المضادات الميكروبية

مضادات البكتيريا

مضادات الفطريات

مضادات الطفيليات

مضادات الفايروسات

علم الخلية

الوراثة

الأحياء العامة

المناعة

التحليلات المرضية

الكيمياء الحيوية

مواضيع متنوعة أخرى

الانزيمات
Joints and Ligaments
المؤلف:
Kelly M. Harrell and Ronald Dudek
المصدر:
Lippincott Illustrated Reviews: Anatomy
الجزء والصفحة:
21-7-2021
3005
Joints and Ligaments
Joints of the lower limb include the hip joint, knee joint, tibiofibular joint, ankle joint, and foot joints.
A. Hip joint
The hip is a synovial, ball-and-socket joint that connects the pelvis to the lower limb (Figs. 1and 2). The head of the femur (ball) and acetabulum (socket) articulate in a deep, protected configuration that still allows for movement in multiple planes. Movements at the joint include flexion, extension, abduction, adduction, medial rotation, lateral rotation, and circumduction. The hip joint is supported by ligamentous and capsular structures.
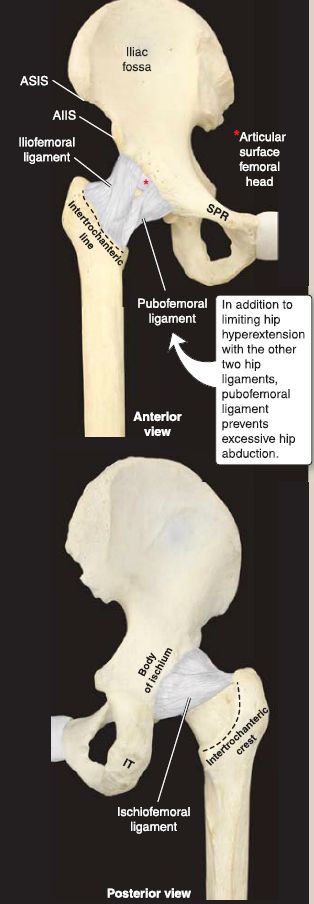
Figure 1:Hip joint and associated supporting structures. AIIS = anterior inferior
iliac spine, ASIS = anterior superior iliac spine, IT = ischial tuberosity, SPR = superior pubic ramus.

Figure 2: Plain film radiograph of normal hip (dotted line-intertrochanteric line). A = acetabulum, NP = anterior/ posterior, GT = greater trochanter, H = head, N = neck, S = shaft.
1. Acetabulum: Articular cartilage lines both the head of the femur and the lunate surface of the acetabulum. A fibrocartilagenous acetabular labrum is attached along the rim of the acetabulum to further deepen the joint.
2. Fibrous capsule: The fibrous capsule of the hip extends from the bony rim of the acetabulum to portions of the femoral neck. Thickenings in the capsule represent hip ligaments.
3. Ligaments: The iliofemoral ligament lies anterior and superior and prevents hyperextension of the hip. The pubofemoral ligament lies inferior and prevents excessive abduction of the hip. The ischiofemoral ligament lies posterior and is the weakest of the three. Collectively, these ligaments assist the medial and lateral hip rotators in maintaining the position of the femoral head in the acetabulum to achieve stability. The ligament of the head of femur assists in the strength of the joint as well.
4. Vasculature: A small and often wanting branch from the obturator artery-artery to the head of the femur-travels through the ligament to supply this region. Medial and lateral circumflex femoral arteries give rise to retinacular arteries, which extend into the capsule and supply the hip joint.
5. Articular innervation: The joint receives innervation from branches of the femoral nerve, obturator nerve, superior gluteal nerve, and nerve to quadratus femoris.
6. Bursae: Three main synovial fluid-filled bursa sacs are associated with the hip and gluteal regions. The trochanteric bursa lies between the deep surface of gluteus maxim us and greater trochanter. The gluteofemoral bursa lies between the proximal iliotibial band and the superior attachment of vastus lateralis. The ischial bursa lies between the inferior border of the gluteus maximus and ischial tuberosity.
B. Knee joint
The knee is a synovial, hinge joint that connects the thigh to the leg (Figs. 3 and 4). The distal femur articulates with both the proximal tibia and patella to allow for movement, primarily in the sagittal plane. Movements at the joint include flexion, extension, and very minimal terminal rotation. The knee joint is supported by ligamentous and capsular structures.
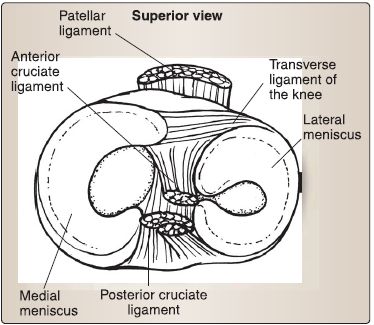
Figure 3: Knee joint.
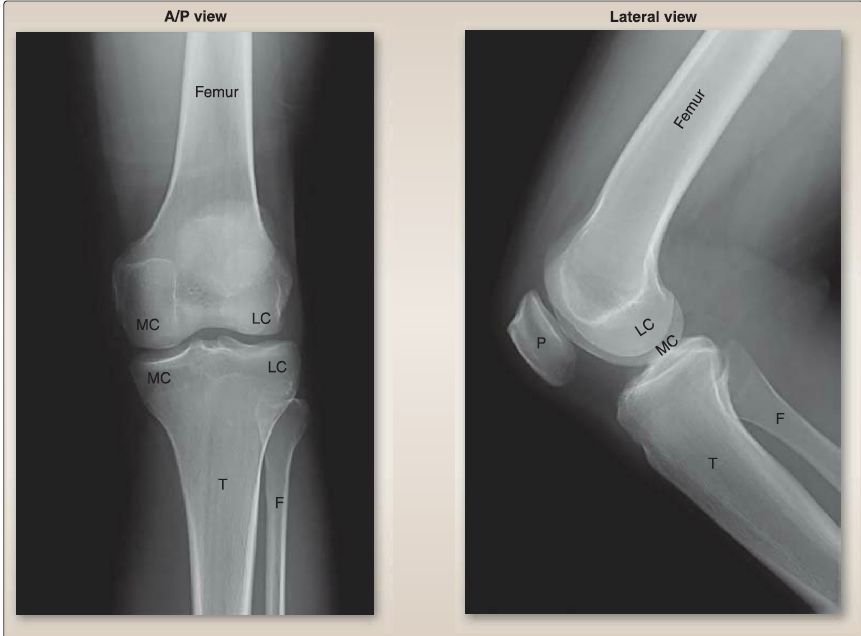
Figure 4: Plain film radiographs of normal knee joint. A/P = anterior/posterior, F = fibula, LC = lateral condyle, MC = medial condyle, P = patella, T = tibia.
1. Cartilage: Articular hyaline cartilage lines both the femoral and tibial condyles and posterior patella. Crescent-shaped fibrocartilagenous plates called menisci (medial and lateral} are attached on the tibial articular surface to further deepen the joint surface and provide shock absorption.
2. Fibrous capsule: The fibrous capsule of the knee extends from the boundaries of the femoral and tibial articular surfaces and is inherently weak posteriorly. An inner synovial layer lines the surfaces of the joint that are void of articular cartilage.
3. Ligaments: Thickenings in the capsule represent the intrinsic knee ligaments (Fig. 5).
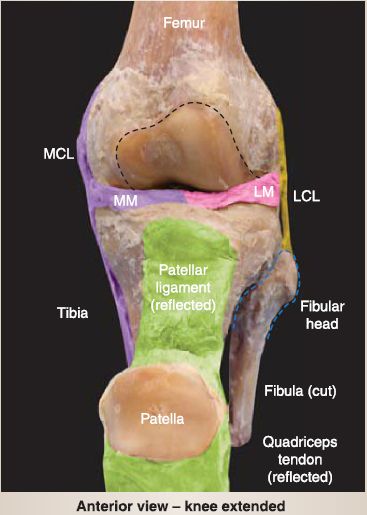
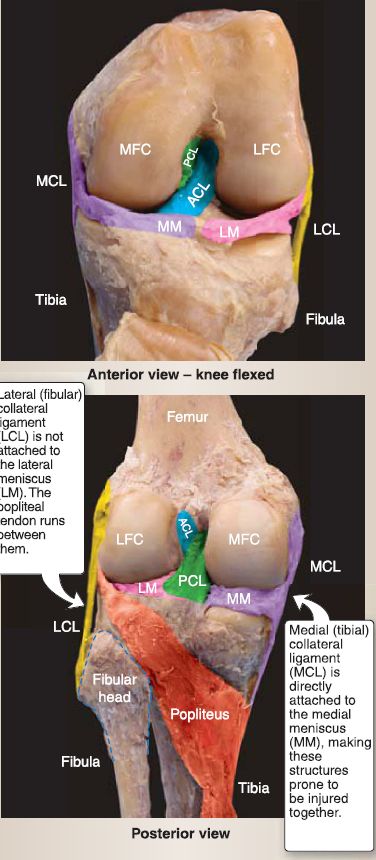
Figure 5: Knee ligaments. AGL = anterior cruciate ligament, LFG = lateral femoral condyle, MFG = medial femoral condyle, PGL = posterior cruciate ligament.
a. Medial (tibial) collateral ligament (MCL): The MCL extends from the medial epicondyle of the femur to the medial condyle and superior surface of tibia. It tightens with valgus force and is attached to the medial meniscus.
b. Patellar ligament: This ligament is a strong, thick extension of the quadriceps tendon. It attaches to the tibial tuberosity.
c. Arcuate popliteal ligament: This ligament arises from the fibular head to support the posterior capsule.
d. Oblique popliteal ligament: This ligament is an extension of the semimembranosus tendon and provides capsular support posteriorly.
e. Lateral (fibular) collateral ligament (LCL): The cord-like LCL further supports the joint capsule but is considered extracapsular. It extends from the lateral epicondyle of the femur to the fibular head and is not directly attached to the lateral meniscus, as the popliteal tendon separates the two structures. The LCL tightens with a varus stress.
f. Anterior cruciate ligament (ACL) and posterior cruciate ligament (PCL): These cross each other deep to the knee joint and limit the rotation at the knee. They lie outside the articular cavity, but within the capsule. The ACL runs from the anterior intercondylar region of the tibia to the posteromedial surface of the lateral femoral condyle. It limits anterior translation of the tibia on the femur (unfixed leg) and hyperextension of the knee.
The PCL is the weaker of the two cruciates and runs from the posterior intercondylar region of the tibia to the anterolateral surface of the medial femoral condyle. It limits posterior translation of the tibia on the femur (unfixed leg) and hyperflexion of the knee.
4. Vasculature: The popliteal artery and vein give rise to geniculate vessels that extend into the capsule and supply the knee joint. 5. Articular innervation: The joint receives innervation from articular branches of the femoral, tibial, common fibular, and obturator nerves.
6. Bursae: Approximately a dozen bursae are associated with the knee region, but only four communicate directly with the articular cavity: The suprapatellar bursa lies deep to the quadriceps tendon, the popliteus bursa lies between the popliteus and lateral tibial condyle, the anserine bursa lies between the pes anserinus (gracilis, sartorius, and semitendinosus tendons) and MCL, and the gastrocnemius bursa lies deep to the medial head of the gastrocnemius.
C. Tibiofibular joint
As shown in Figure 6, the tibiofibular joint is a syndesmosis fibrous joint held together by an interosseous membrane that spans between the tibial and fibular shafts as well as distal tibiofibular ligaments (anterior, interosseous, and posterior). The collection of distal tibiofibular ligaments provides additional support to maintain the integrity of the ankle joint. Trace movement occurs at the distal end of this joint during ankle dorsiflexion. Branches from the fibular artery and anterior and posterior tibial arteries supply this joint, while innervation is mediated by branches of the tibial, deep fibular, and saphenous nerves.
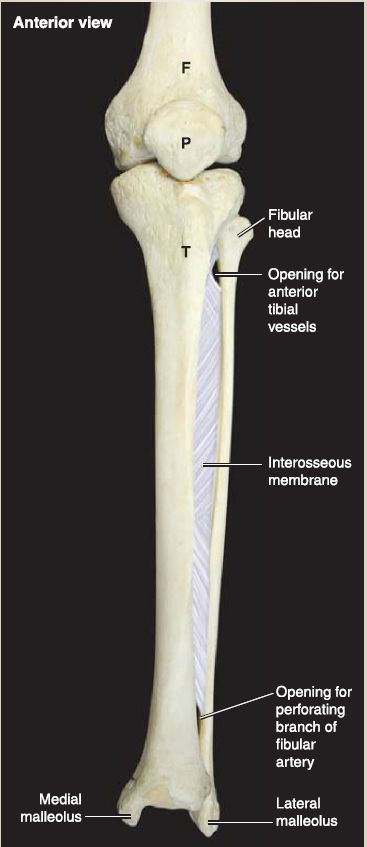
Figure 6: Tibiofibular joint. F = femur, P = patella, T = tibia.
D. Ankle joint
As shown in Figures 7 and 8, the ankle joint is composed of the distal tibia and fibula articulating with the superior articular surface of the talus.
1. Movement: This joint allows only flexion and extension movement in the sagittal plane. All other foot movements (eversion, inversion, rotation) occur in the subtalar regions.
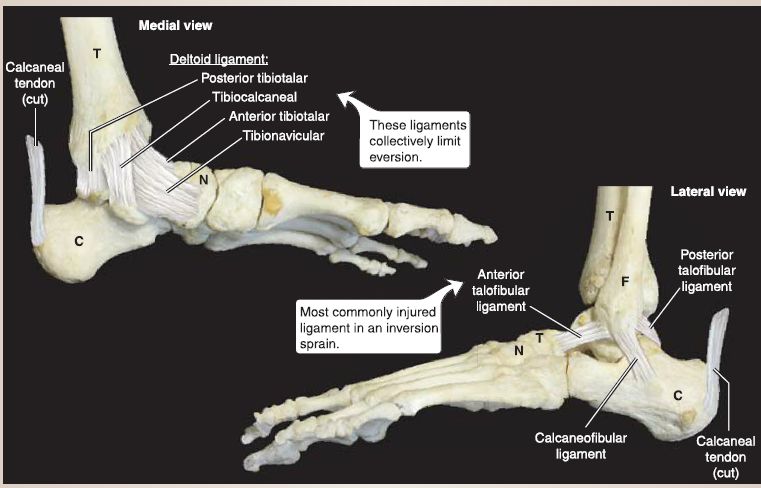
Figure 7: Ankle joint. C = calcaneus, F = fibula, N = navicular, T = tibia.
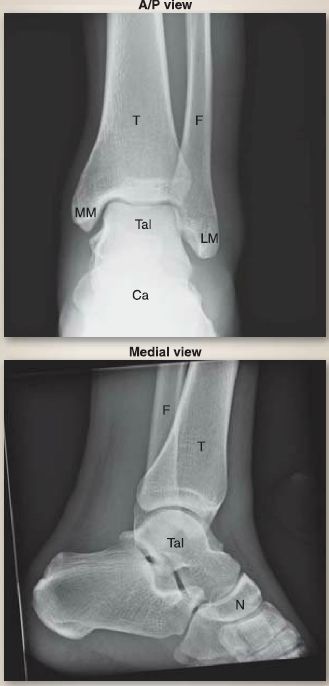
Figure 8: Plain film radiographs of normalankle. A/P = anterior/posterior, Ca = calcaneus, F = fibula, LM = lateral malleolus, MM = medial malleolus, N = navicula, T = tibia, Tai= talus.
2. Ligaments: The ankle joint is supported medially by the strong fan-shaped deltoid ligament, which consists of the tibionavicular part, tibiocalcaneal part, and the anterior and posterior tibiotalar parts. This collection of ligaments resists eversion of the ankle joint. Laterally, the ankle is supported by the anterior and posterior talofibular ligaments and the calcaneofibular ligament. Collectively, these ligaments resist inversion, but they are weaker than their medial counterparts.
3. Vasculature: Malleolar branches from the posterior and anterior tibial and fibular arteries supply the ankle joint.
4. Articular innervation: Ankle joint innervation is mediated by branches of the deep fibular and tibial nerves.
E. Foot joints
Joints of the foot are numerous and include the subtalar, talocalcaneonavicular, calcaneocuboid, cuneonavicular, tarsometatarsal, intermetatarsal, metatarsophalangeal, and interphalangeal joints (Fig. 9). Figure 10 shows plain film of the foot and bones.
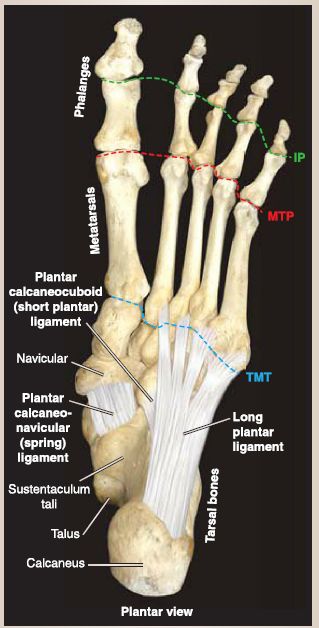
Figure 9: Foot joints. Supporting ligamentous structures. IP = interphalangeal joints,
MTP = metatarsophalangeal joints, TMT = tarsometatarsal joint.
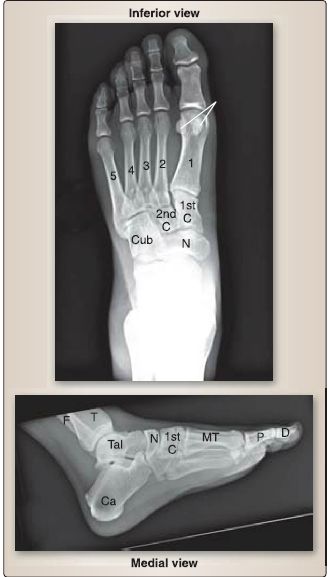
Figure 10 : Plain film radiographs of normal foot. C = cuneiform, Ca = calcaneus, Cub = cuboid, D = distal phalange, F = fibula, MT= metatarsals (1-5), N = navicula,P = proximal phalange, T = tibia, Tai = talus.
1. Movement: Owing to the multiplane nature of the foot, interarticular movements include inversion, aversion, gliding, rotation, sliding, circumduction, flexion, extension, abduction, and adduction. These articulations allow the foot to adjust to changes in the ground and transmit forces superiorly through the kinetic chain during the gait cycle. The subtalar joint is a plane synovial articulation between the talus and calcaneus where most of the aversion and inversion occurs. The calcaneocuboid joint also contributes to aversion and inversion. Flexion, extension, abduction, and adduction occur at the metatarsophalangeal joints, whereas interphalangeal joints allow for flexion and extension only.
2. Ligaments: Major supporting ligaments of the foot include the plantar calcaneonavicular ligament (spring ligament), long plantar ligament, and the short plantar ligament (plantar calcaneocuboid ligament). These ligaments passively support the longitudinal and transverse arches of the foot.
3. Vasculature: Branches from dorsalis pedis and MP and LP arteries give rise to tarsal and digital arteries to supply the foot and toes.
4. Articular innervation: Collectively, joints of the foot receive innervation from articular branches of the MP and LP nerves and the deep fibular nerves. Digital branches serve the toes.
 الاكثر قراءة في علم التشريح
الاكثر قراءة في علم التشريح
 اخر الاخبار
اخر الاخبار
اخبار العتبة العباسية المقدسة

الآخبار الصحية












 قسم الشؤون الفكرية يصدر كتاباً يوثق تاريخ السدانة في العتبة العباسية المقدسة
قسم الشؤون الفكرية يصدر كتاباً يوثق تاريخ السدانة في العتبة العباسية المقدسة "المهمة".. إصدار قصصي يوثّق القصص الفائزة في مسابقة فتوى الدفاع المقدسة للقصة القصيرة
"المهمة".. إصدار قصصي يوثّق القصص الفائزة في مسابقة فتوى الدفاع المقدسة للقصة القصيرة (نوافذ).. إصدار أدبي يوثق القصص الفائزة في مسابقة الإمام العسكري (عليه السلام)
(نوافذ).. إصدار أدبي يوثق القصص الفائزة في مسابقة الإمام العسكري (عليه السلام)