

النبات

مواضيع عامة في علم النبات

الجذور - السيقان - الأوراق

النباتات الوعائية واللاوعائية

البذور (مغطاة البذور - عاريات البذور)

الطحالب

النباتات الطبية


الحيوان

مواضيع عامة في علم الحيوان

علم التشريح

التنوع الإحيائي

البايلوجيا الخلوية


الأحياء المجهرية

البكتيريا

الفطريات

الطفيليات

الفايروسات


علم الأمراض

الاورام

الامراض الوراثية

الامراض المناعية

الامراض المدارية

اضطرابات الدورة الدموية

مواضيع عامة في علم الامراض

الحشرات


التقانة الإحيائية

مواضيع عامة في التقانة الإحيائية


التقنية الحيوية المكروبية

التقنية الحيوية والميكروبات

الفعاليات الحيوية

وراثة الاحياء المجهرية

تصنيف الاحياء المجهرية

الاحياء المجهرية في الطبيعة

أيض الاجهاد

التقنية الحيوية والبيئة

التقنية الحيوية والطب

التقنية الحيوية والزراعة

التقنية الحيوية والصناعة

التقنية الحيوية والطاقة

البحار والطحالب الصغيرة

عزل البروتين

هندسة الجينات


التقنية الحياتية النانوية

مفاهيم التقنية الحيوية النانوية

التراكيب النانوية والمجاهر المستخدمة في رؤيتها

تصنيع وتخليق المواد النانوية

تطبيقات التقنية النانوية والحيوية النانوية

الرقائق والمتحسسات الحيوية

المصفوفات المجهرية وحاسوب الدنا

اللقاحات

البيئة والتلوث


علم الأجنة

اعضاء التكاثر وتشكل الاعراس

الاخصاب

التشطر

العصيبة وتشكل الجسيدات

تشكل اللواحق الجنينية

تكون المعيدة وظهور الطبقات الجنينية

مقدمة لعلم الاجنة


الأحياء الجزيئي

مواضيع عامة في الاحياء الجزيئي


علم وظائف الأعضاء


الغدد

مواضيع عامة في الغدد

الغدد الصم و هرموناتها

الجسم تحت السريري

الغدة النخامية

الغدة الكظرية

الغدة التناسلية

الغدة الدرقية والجار الدرقية

الغدة البنكرياسية

الغدة الصنوبرية

مواضيع عامة في علم وظائف الاعضاء

الخلية الحيوانية

الجهاز العصبي

أعضاء الحس

الجهاز العضلي

السوائل الجسمية

الجهاز الدوري والليمف

الجهاز التنفسي

الجهاز الهضمي

الجهاز البولي


المضادات الميكروبية

مواضيع عامة في المضادات الميكروبية

مضادات البكتيريا

مضادات الفطريات

مضادات الطفيليات

مضادات الفايروسات

علم الخلية

الوراثة

الأحياء العامة

المناعة

التحليلات المرضية

الكيمياء الحيوية

مواضيع متنوعة أخرى

الانزيمات
Amino acids : Conversion to Specialized Products
المؤلف:
Denise R. Ferrier
المصدر:
Lippincott Illustrated Reviews: Biochemistry
الجزء والصفحة:
16-11-2021
1250
Amino acids : Conversion to Specialized Products
Amino acids are precursors of many nitrogen (N)-containing compounds including porphyrins, which, in combination with ferrous (Fe2+) iron, form heme (Fig. 1). The major sites of heme biosynthesis are the liver, which synthesizes a number of hemeproteins (particularly cytochrome P450 enzymes), and the erythrocyte-producing cells of the bone marrow, which are active in hemoglobin synthesis. In the liver, the rate of heme synthesis is highly variable, responding to alterations in the cellular heme pool caused by fluctuating demands for hemeproteins.
In contrast, heme synthesis in erythroid cells is relatively constant and is matched to the rate of globin synthesis. Heme synthesis starts with glycine and succinyl coenzyme A. The committed step is the formation of δ-aminolevulinic acid (ALA). This mitochondrial reaction is catalyzed by ALA synthase-1 (ALAS1) in the liver (inhibited by hemin, the oxidized form of heme that accumulates when heme is being underutilized) and ALAS2 in erythroid tissues (regulated by iron). Porphyrias are caused by inherited or acquired (lead poisoning) defects in heme synthesis, resulting in the accumulation and increased excretion of porphyrins or porphyrin precursors. Enzymic defects early in the pathway cause abdominal pain and neuropsychiatric symptoms, whereas later defects cause photosensitivity.
Degradation of heme occurs in the mononuclear phagocyte system, particularly in the liver and spleen. The first step is the production by heme oxygenase of biliverdin, which is subsequently reduced to bilirubin. Bilirubin is transported by albumin to the liver, where its solubility is increased by the addition of two molecules of glucuronic acid by bilirubin uridine diphosphate-glucuronosyltransferase (bilirubin UGT). Bilirubin diglucuronide (conjugated bilirubin) is transported into the bile canaliculi, where it is first hydrolyzed and reduced by gut bacteria to yield urobilinogen, which is further oxidized by bacteria to stercobilin. Jaundice (icterus) refers to the yellow color of the skin and sclerae that is caused by deposition of bilirubin, secondary to increased bilirubin levels in the blood.
Three commonly encountered types of jaundice are hemolytic (prehepatic), obstructive (posthepatic), and hepatocellular (hepatic) (see Fig. 1). Other important N-containing compounds derived from amino acids include the catecholamines (dopamine, norepinephrine, and epinephrine), creatine, histamine, serotonin, melanin, and nitric oxide.
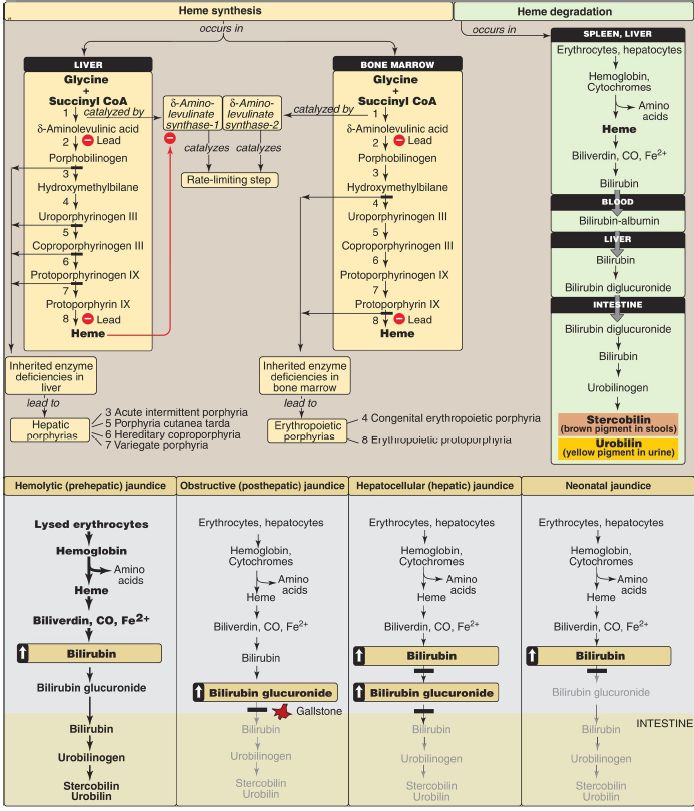
Figure 1: Key concept map for heme metabolism. = Block in the pathway. [Note: Hepatocellular jaundice can be caused by decreased conjugation of bilirubin or decreased secretion of conjugated bilirubin from the liver into bile.] CoA = coenzyme A; CO = carbon monoxide; Fe = iron.
 الاكثر قراءة في الكيمياء الحيوية
الاكثر قراءة في الكيمياء الحيوية
 اخر الاخبار
اخر الاخبار
اخبار العتبة العباسية المقدسة

الآخبار الصحية















 قسم الشؤون الفكرية يصدر كتاباً يوثق تاريخ السدانة في العتبة العباسية المقدسة
قسم الشؤون الفكرية يصدر كتاباً يوثق تاريخ السدانة في العتبة العباسية المقدسة "المهمة".. إصدار قصصي يوثّق القصص الفائزة في مسابقة فتوى الدفاع المقدسة للقصة القصيرة
"المهمة".. إصدار قصصي يوثّق القصص الفائزة في مسابقة فتوى الدفاع المقدسة للقصة القصيرة (نوافذ).. إصدار أدبي يوثق القصص الفائزة في مسابقة الإمام العسكري (عليه السلام)
(نوافذ).. إصدار أدبي يوثق القصص الفائزة في مسابقة الإمام العسكري (عليه السلام)


















