

النبات

مواضيع عامة في علم النبات

الجذور - السيقان - الأوراق

النباتات الوعائية واللاوعائية

البذور (مغطاة البذور - عاريات البذور)

الطحالب

النباتات الطبية


الحيوان

مواضيع عامة في علم الحيوان

علم التشريح

التنوع الإحيائي

البايلوجيا الخلوية


الأحياء المجهرية

البكتيريا

الفطريات

الطفيليات

الفايروسات


علم الأمراض

الاورام

الامراض الوراثية

الامراض المناعية

الامراض المدارية

اضطرابات الدورة الدموية

مواضيع عامة في علم الامراض

الحشرات


التقانة الإحيائية

مواضيع عامة في التقانة الإحيائية


التقنية الحيوية المكروبية

التقنية الحيوية والميكروبات

الفعاليات الحيوية

وراثة الاحياء المجهرية

تصنيف الاحياء المجهرية

الاحياء المجهرية في الطبيعة

أيض الاجهاد

التقنية الحيوية والبيئة

التقنية الحيوية والطب

التقنية الحيوية والزراعة

التقنية الحيوية والصناعة

التقنية الحيوية والطاقة

البحار والطحالب الصغيرة

عزل البروتين

هندسة الجينات


التقنية الحياتية النانوية

مفاهيم التقنية الحيوية النانوية

التراكيب النانوية والمجاهر المستخدمة في رؤيتها

تصنيع وتخليق المواد النانوية

تطبيقات التقنية النانوية والحيوية النانوية

الرقائق والمتحسسات الحيوية

المصفوفات المجهرية وحاسوب الدنا

اللقاحات

البيئة والتلوث


علم الأجنة

اعضاء التكاثر وتشكل الاعراس

الاخصاب

التشطر

العصيبة وتشكل الجسيدات

تشكل اللواحق الجنينية

تكون المعيدة وظهور الطبقات الجنينية

مقدمة لعلم الاجنة


الأحياء الجزيئي

مواضيع عامة في الاحياء الجزيئي


علم وظائف الأعضاء


الغدد

مواضيع عامة في الغدد

الغدد الصم و هرموناتها

الجسم تحت السريري

الغدة النخامية

الغدة الكظرية

الغدة التناسلية

الغدة الدرقية والجار الدرقية

الغدة البنكرياسية

الغدة الصنوبرية

مواضيع عامة في علم وظائف الاعضاء

الخلية الحيوانية

الجهاز العصبي

أعضاء الحس

الجهاز العضلي

السوائل الجسمية

الجهاز الدوري والليمف

الجهاز التنفسي

الجهاز الهضمي

الجهاز البولي


المضادات الميكروبية

مواضيع عامة في المضادات الميكروبية

مضادات البكتيريا

مضادات الفطريات

مضادات الطفيليات

مضادات الفايروسات

علم الخلية

الوراثة

الأحياء العامة

المناعة

التحليلات المرضية

الكيمياء الحيوية

مواضيع متنوعة أخرى

الانزيمات
Coeliac disease
المؤلف:
James Carton
المصدر:
Oxford Handbook of Clinical Pathology 2024
الجزء والصفحة:
3rd edition , p122-123
2025-02-09
757
Definition
• An autoimmune disorder caused by an abnormal immune response to dietary gluten.
Epidemiology
• Common, affecting ~1% of the population.
Aetiology
• Dietary gluten and related proteins.
Pathogenesis
• the culprit proteins are poorly digested by intestinal proteases.
• Intact peptides enter the lamina propria and are deamidated by tissue transglutaminase, rendering them negatively charged.
• Negatively charged peptides bind more efficiently to human leucocyte antigen (HLA) receptors on antigen- presenting cells which are recognized by intestinal T- cells.
• Activated T- cells stimulate an immune reaction in the intestinal wall.
Presentation
• Symptoms relating to the GI tract may be present such as weight loss, abdominal pain, and diarrhoea.
• however, many patients are asymptomatic and only diagnosed during investigation of an iron deficiency anaemia.
Serology
• Presence of serum IgA endomysial or transglutaminase antibodies is highly specific and sensitive for coeliac disease. Care must be taken in interpreting these results in patients who are IgA- deficient.
Macroscopy
• Blunting and flattening of villi may be visible under a dissecting microscope (and may be identified at endoscopy).
Histopathology
• fully developed cases show increased intraepithelial lymphocytes (>20/ 100 epithelial cells), mainly at the tips of the villi, many lymphocytes and plasma cells in the lamina propria, villous atrophy, and crypt hyperplasia (fig. 1).
• Milder cases may only show increased intraepithelial lymphocytes without villous atrophy. this is termed lymphocytic duodenitis.
* Note that none of these changes are specific to coeliac disease; identical changes can be seen in a number of other conditions, e.g. drugs, tropical sprue. Biopsy findings must be interpreted in light of the clinical and serological picture.
Prognosis
• Strict adherence to a gluten- free diet leads to resolution of symptoms and normalization of histology, although architectural changes may take some time to normalize. Cases which do not respond to a gluten- free diet need to be carefully assessed for the development of a lymphoma.
• Increased risk of type 1 diabetes, autoimmune thyroid disease, dermatitis herpetiformis, oropharyngeal and oesophageal carcinomas, small bowel adenocarcinoma, and a rare, but highly aggressive, form of t- cell lymphoma known as enteropathy- associated t- cell lymphoma (EATL).
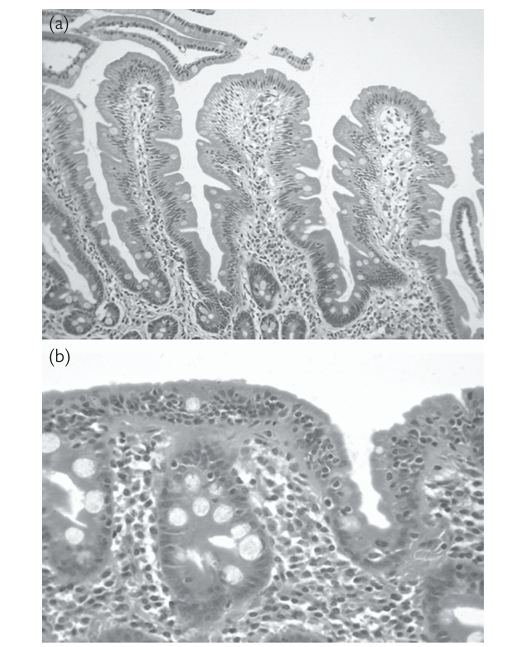
FIG1. (a) Normal duodenal mucosa. the villi have a normal height and shape, and there is no increase in intraepithelial lymphocytes. (b) Duodenal biopsy from a patient with gluten- sensitive enteropathy. the villi have completely disappeared and the surface epithelium contains many intraepithelial lymphocytes . reproduced with permission from Clinical Pathology (Oxford Core texts), Carton, James, Daly, richard, and ramani, Pramila, Oxford University Press (2006), p.154, figure 8.8.
 الاكثر قراءة في الامراض المناعية
الاكثر قراءة في الامراض المناعية
 اخر الاخبار
اخر الاخبار
اخبار العتبة العباسية المقدسة

الآخبار الصحية















 قسم الشؤون الفكرية يصدر كتاباً يوثق تاريخ السدانة في العتبة العباسية المقدسة
قسم الشؤون الفكرية يصدر كتاباً يوثق تاريخ السدانة في العتبة العباسية المقدسة "المهمة".. إصدار قصصي يوثّق القصص الفائزة في مسابقة فتوى الدفاع المقدسة للقصة القصيرة
"المهمة".. إصدار قصصي يوثّق القصص الفائزة في مسابقة فتوى الدفاع المقدسة للقصة القصيرة (نوافذ).. إصدار أدبي يوثق القصص الفائزة في مسابقة الإمام العسكري (عليه السلام)
(نوافذ).. إصدار أدبي يوثق القصص الفائزة في مسابقة الإمام العسكري (عليه السلام)


















